This year is shaping up to be a consequential moment for the future of drug pricing in the United States—especially for young Americans.
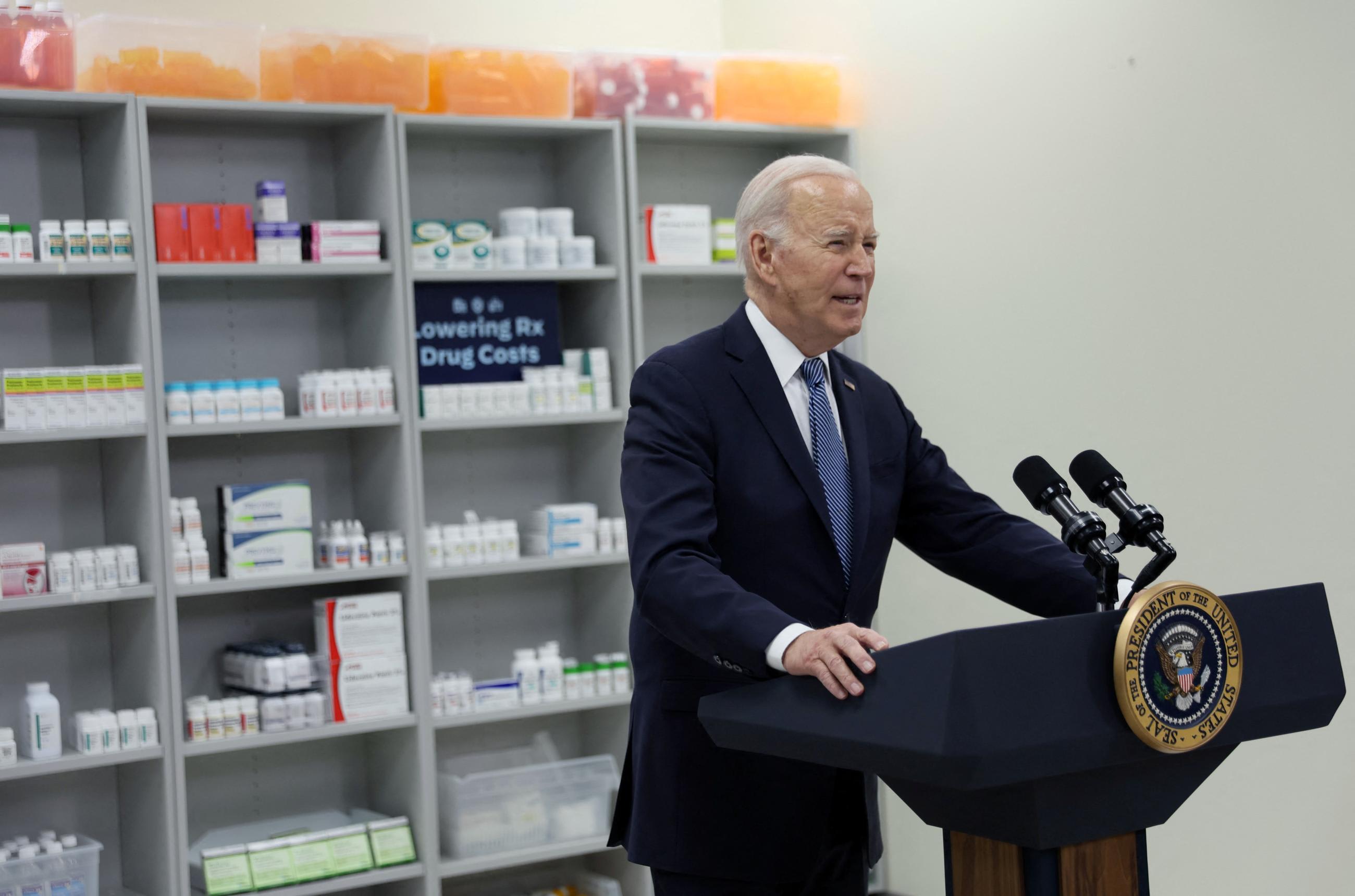
In 2022, the Joe Biden administration passed landmark national legislation to lower drug prices for seniors as part of the Inflation Reduction Act (IRA). The move was a major step forward in a long-fought battle over prescription drug prices, which, on average, are nearly three times those of other countries, according to RAND.
The law allows the Department of Health and Human Services to undercut the drug pricing supply chain, authorizing it to negotiate directly with manufacturers for lower prices for the most expensive drugs for people with Medicare. Provisions in effect as of January have already led companies to lower the price of insulin to just $35 for Medicare beneficiaries.
Originally the policy was to apply to everyone with health insurance, but Republicans in the Senate demanded that it apply only to older adults—leaving young people behind. Still, advocates are hopeful that the IRA will have a ripple effect for affordability for other patient demographics.
"This is a really transformative first step," said Sneha Dave, founder of the advocacy organization Generation Patient. "And there's going to be so much more that comes."
Currently, 1 in 4 Americans report difficulty affording their medication, which in turn harms their health. When uninsured or underinsured individuals rely on expensive drugs to manage a disease, they are more likely to skip or delay doses and to factor those costs into their ability to afford basic needs such as food or housing.
For young adults with chronic conditions, those decisions threaten to shape the course of their lives.
U.S. Drug Prices Overshadow Those in Other Countries
Americans pay a greater share of their budgets for prescription drugs, with brand-name drugs being the most costly
"Our demographic is one of the most financially unstable, and to add prescription medications into that is challenging," said Dave. "The decisions we make are very much centered around our ability to afford medications into the future."
Due to advances in modern medicine, 90 to 95% of children diagnosed with chronic illnesses such as diabetes, lupus, and juvenile arthritis survive to adulthood. Still, those young people carry a higher risk of hospitalization and often rely on medication for life. No low-cost generic medications are available for many of those illnesses, and for people with multiple conditions, paying for multiple prescription drugs can be exorbitant. Many young people are also transitioning insurance or losing their parents' coverage, leading them to pay more out-of-pocket.
A quarter of Americans report difficulty affording their medication, which in turn harms their health
"We are seeing an influx of patients entering the medical system for chronic conditions, and more and more of us are being diagnosed at younger ages." said Dave. "It's critical for us to be thinking about not only the challenges on the individual level of navigating life and various systems with a chronic illness, but also thinking systemically what the barriers exist for us to be able to thrive into adulthood."
A Uniquely American System
Prescription drug spending in the United States increased by 91% from 2000 to 2020. The pharmaceutical industry still has the largest profit margins among publicly traded companies of any sector, including tech. The decision-making process behind price-setting is murky and not fully explained by investments in research and development. In other countries where those prices are negotiated, the same drugs created by the same companies cost a fraction of U.S. prices.
Drug Spending on the Rise
The United States spent $603 billion on prescription drugs in 2021, largely driven by high-cost specialty drugs
"The initial prices for branded drugs are currently much higher than those in other countries," said Andrew Mulcahy, senior health economist at RAND. "And the magnitude of that comparison really depends on whether you're talking brand or generic drugs—[prices] are all over the place."
Before reaching the patient, a drug passes through a supply chain, each step of which plays a role in determining its final price. Pharmaceutical companies make the first move, setting an initial list price for the medications they manufacture. Later, pharmacy benefit managers (PBMs), companies contracted by a health plan, negotiate a discount with the manufacturer. As part of the negotiation, they receive a rebate, part of which is passed along to insurers.
Because PBMs receive a larger rebate for more expensive drugs, some cases may carry an incentive to favor higher-priced drugs over cheaper ones. In turn, pharmaceutical companies sometimes price drugs higher to account for larger rebates. Advocates and lawmakers have cited rebates as a major driver of high—and growing—list prices for brand-name insulin, which were nearly 10 times higher in the United States than in other countries, according to RAND.
Final prices are also shaped by discounts through Medicaid, the 340B prescription drug discount program and other sources.
"We find that even after taking [discounts] into account, prices remain high." said Mulcahy. "If you don't have insurance, if you're underinsured—that initial price really matters."
Prices are also kept high due to anticompetitive practices for brand-name drugs, such as patent thickets, product hopping, and pay-for-delay, which extend lucrative patents and make it challenging for generics and biosimilars to enter the market.
For far too long patient groups have been left behind in engaging in the patent system
Sneha Dave, founder, Generation Patient
RAND's recent report found that the availability of generics is a silver lining: Even though brand-name drug prices continue to climb, the cost of generics in the United States is about 67% that in other countries. Because generics are so much more affordable, reforming the patent system is a top priority for advocates.
"Making sure that we close some of those loopholes that exist for companies to abuse the patent system is really crucial," said Dave. "For far too long patient groups have been left behind in engaging in the patent system. In some ways, it's designed to be complex, and to leave the public out."
What's Fair?
Eleven states, including Colorado, Maryland, and New York, have already followed the IRA's lead by creating Prescription Drug Affordability Boards (PDAB) to curb costs for certain drugs. Thirteen more states have pending legislation to establish their own PDABs.
The changes signal a major shift toward transparency and engagement with the drug pricing process as well as in how Americans view health care.
PDABs echo Europe's Health Technology Assessment Bodies, which work with regulators to determine a fair price for a particular prescription medication. These bodies emphasize that access to medicines is necessary for public health.
"The United States has a focus on savings and value from a payor perspective, not the broader societal perspective," said Mulcahy. "In the United States, 'fair prices' are the outcome of negotiations. Other countries get a sense of what's fair from value [to society]."
The IRA cites research and development costs, costs of production and distribution, and sales data among factors for determining a final "fair price."
Advocates hope that patients will have a greater say in defining what's fair. With her advocacy organization Generation Patient, Sneha Dave has spoken at the White House, served on the Democratic National Committee Disability Policy Subcommittee, and forms part of a patient engagement collaborative for the Food and Drug Administration.
"We know the power of lived experience in driving a lot of health policy decisions," said Dave. "So we hope that that is only amplified and included in key health policy issues."