"There is a golden hour between life and death."
In the early 1980s, R. Adam Cowley, a U.S. military surgeon popularized the term "golden hour," words often used in trauma and emergency medicine settings. The term's origins lie in photography and reference the first hour of light after the sun rises and the last hour of light before sunset. That concept of a critical window of perfect sunlight was co-opted by emergency medical providers to refer to the crucial period of time immediately after an injury when appropriate life-saving medical or surgical intervention can offer the highest chance of survival for a traumatically injured patient.
There is a crucial period immediately after an injury when life-saving medical or surgical intervention can offer the highest chance of survival
Although there is little scientific basis for this traditional one-hour rule, as many trauma care providers note, trauma care is time-dependent and a prompt response can be a matter of life and death. The "golden hour" is now more scientifically referred to as the "resuscitative hour."
In much of the world, road traffic accident victims and others suffering life-threatening injuries are not able to receive essential surgical care—including trauma, surgery, and anesthesia care—within an hour, or even many hours, following an accident. The window of opportunity for a chance at survival is narrow for a severely injured patient. Road traffic and other injuries kill more people every year than HIV-AIDS, tuberculosis, and malaria combined. Though injury-related deaths occur everywhere, the overwhelming majority happen in low- and middle-income countries (LMICs), where emergency communication systems and health care are often limited. Specialized and timely trauma care in LMICs is critical, though, to reducing permanent, long-term disability and deaths.
COVID-19 Lockdowns and Traffic Accidents
During the COVID pandemic, the world initially witnessed a dip in the volume of injuries presenting to emergency departments—a phenomenon linked to restricted travel. A global review indicated that there was a worldwide reduction of between 20.3 percent and 84.6 percent in trauma patients [treated in health-care facilities] compared to a pre-COVID control period. The reduction in traumatic injuries did not, however, translate to reductions in the severity and kinds of injuries seen. In turn, the need for both acute trauma care and for longer term rehabilitation services did not decrease, and it has remained critical throughout the COVID-19 pandemic.
Although the overall trauma case volume—especially due to road traffic accidents—decreased during lockdowns, injuries due to road traffic accidents may, in some instances, have been of higher severity. In the United States, the pandemic significantly reduced traffic volume, but the rate of traffic fatalities per miles driven jumped by 18 percent in 2020, according to the National Highway Traffic Safety Administration. Safety experts have blamed speeding on emptier roads for the increase in traffic fatalities. Japan reported a similar narrative.
In some LMICs, where the "informal economy" is critical to day-to-day survival for much of the population (those most at risk of traumatic injury), authorities had difficulty enforcing lockdowns effectively. India, for example, did not experience a decrease in the severity of road traffic accidents.
Unmet Need
Even before the pandemic, the delivery of timely, high-quality trauma care was often an unmet need in LMICs. Unlike health systems in high-income countries (HICs) that could, for the most part, continue to maintain functional emergency departments despite pressures of treating COVID-19 patients, and sometimes divert trauma cases to "COVID-free" hospitals, fragile health systems in LMICs often crumbled under the weight of the pandemic.
Middle-income countries, including Mexico and Costa Rica, have reported an ongoing shortage of hospital and intensive care unit (ICU) beds since the start of the pandemic. In Costa Rica, in May 2021, there was a 121 percent excess in occupancy of ICU beds due to COVID-19 patients, leaving critically ill patient—including those suffering from traumatic, life-threatening injuries—without care. Two months later, Mexico faced a similar problem. According to the Mexican Institute of Social Security (IMSS) 52 percent of 7,017 existing beds with oxygen were occupied by COVID-19 patients. Both countries are among those with some of the highest burden of road traffic injuries.

Global Impact of Road Traffic Accidents
Approximately 1.35 million people die each year as a result of road traffic accidents. Between 20 and 50 million additional victims suffer non-fatal injuries, and more than 93 percent of road traffic fatalities occur in LMICs. The health systems are now tasked with the challenges of prolonged delays in the delivery of trauma care, and consequently, higher trauma-related morbidity and mortality rates. The redistribution and task shifting of workforce and resources required to care for COVID cases is a heavy burden with a grave cost—preventable trauma deaths.
The reduction of trauma-related preventable deaths is a UN target. The UN Sustainable Development Goal 3.6 aims to halve all road-related deaths by 2030. Building safer roads and incentivizing safer driving, and creating access to definitive care, are critical to achieving this target.
The UN Sustainable Development Goal 3.6 aims to halve all road-related deaths by 2030
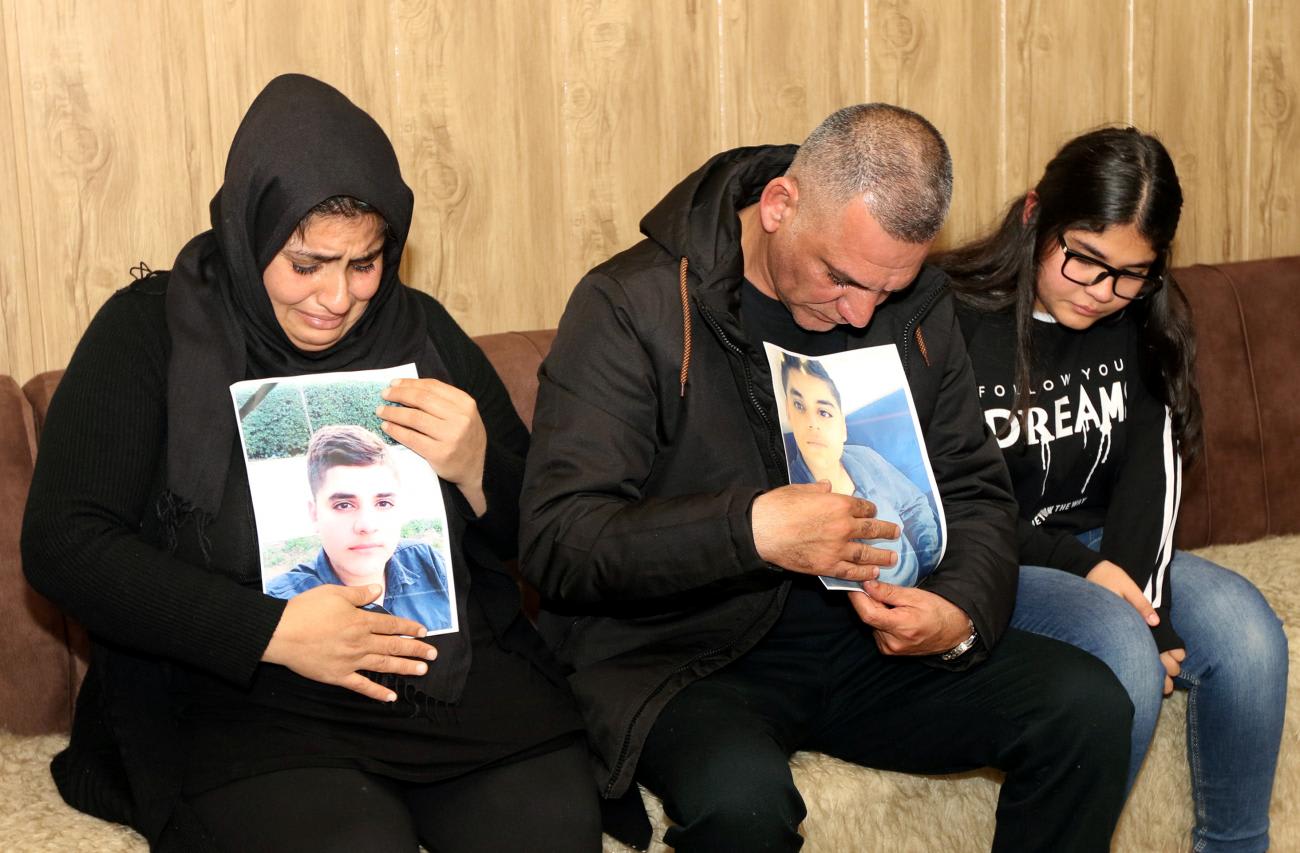
Initiatives to reduce trauma-related injuries must target younger people. Among 5- to 29-year-olds, trauma-related injuries are the leading cause of death. As the recently released documentary Trauma Healers vividly shows, more than half of all road traffic deaths are among pedestrians, cyclists, and motorcyclists—not automobile drivers.
By investing in injury prevention and quality trauma care, countries can mitigate the significant negative economic impact of trauma injuries. An estimated 3 percent of gross domestic product globally is lost due to trauma, including an estimated 1 to 2 percent in HICs and up to 30 percent in LMICs. The rehabilitation of injured patients and their ability to return to work is critical to countries' economies. No country is immune. Countries that have effective trauma care systems, such as the U.K. and Australia, suffer less economic burden due to trauma.
Trauma systems must also be strengthened to avoid the consequential delays in delivering trauma care in the midst of required surge capacity, which COVID continues to make painstakingly clear. Our starting point must be to overcome the barriers to trauma care, including a lack of infrastructure to deliver safe, affordable, and timely care; health workforce shortages; lack of information and communication networks; and improvement of roads and other infrastructures that facilitate geographic access to care.

Reducing Preventable Deaths—a Call to Action
Reducing preventable deaths due to road traffic accidents and providing timely, safe trauma care requires a comprehensive approach that tackles both injury prevention and trauma care delivery. The world has made systematic progress, but there are still significant barriers.
Countries should develop, budget for, and implement national surgical system strengthening plans that are integrated into national health systems strengthening strategies. Strengthening the surgical and anesthesia care systems needed for trauma care can build a country's health system resilience and capacity to respond to pandemics and other health crises. Countries, including LMICs, and donor agencies need to uphold their global commitments to invest in the health sector in general—and in surgical systems in particular. In 2021, for example, the U.S. Congress mandated USAID to invest in strengthening surgical systems, and discussions are underway to attach a funding commitment to this language.
Governments, civil society, and the private sector need to work together to provide safer roads and quality trauma care
Until recently, there was no coordinated research or funding strategy to support the development of surgical care in LMICs such as that which exists with Global Alliance for Vaccines and Immunizations (GAVI) and the Global Fund for HIV, Malaria and Tuberculosis. In early 2020, the Global Surgery Foundation (the GSF), embedded within the UN system, was created as a common platform to pool resources, following the model of other multinational initiatives. The GSF is working to engage with the private sector and multilateral agencies and national governments.
In recognition of the contributions of health workers to the COVID-19 response, 2021 has been declared by the World Health Organization, as the Year of the Health and Care Worker. Even prior to the COVID-19 pandemic, many countries faced pre-existing health workforce challenges, including shortages estimated at 18 million globally, mostly in LMICs, and maldistribution and misalignment of needs and skills. The pandemic has further affected the availability and capacity of health workers to preserve continuity of essential services, including trauma care. More highly skilled health workers are urgently needed, especially in poorer countries, to offer emergency medicine and other trauma-related care, as well as COVID-19 care and other primary health care services.
Civil society organizations and other stakeholders need to continue to support investments in preventing injuries, including road traffic accidents. Without attention to prevention—including safer roads and motor vehicles, along with incentivizing safer driving—national health systems and the world cannot meet the continuing growing need for timely, high-quality, and affordable trauma care. Coalitions such as the Global Alliance for Surgical, Obstetric, Trauma, and Anesthesia Care (The G4 Alliance) and the Global Alliance of NGOs for Road Safety play important roles in raising public awareness and advocating to policy makers for evidence-based policies and resources.
Governments, civil society, and the private sector need to work together to provide safer roads and quality trauma care. Reducing preventable disability and death due to road traffic accidents, and ensuring that emergency and longer-term trauma care and rehabilitation are available and affordable, requires a comprehensive approach that tackles both injury prevention and trauma care delivery capacity.













