When Angelo State University leaders introduced masking mandates at the beginning of the COVID-19 pandemic, Professor Kevin Garrison wrote to his administration: "What the hell are the deaf and hard-of-hearing supposed to do in a world where lips can no longer be read?"
Garrison's experience is similar to that of many hard-of-hearing people who navigate a world now characterized by social distancing, mask-wearing, and fragmented communication. It demonstrates how important it is to consider how COVID-prevention policies and public health recommendations have disproportionately affected the social well-being of hard-of-hearing people.
Prior to the COVID-19 pandemic, hearing loss was already linked to social isolation throughout life, and research shows it can produce emotions such as stress and anger. However, COVID-19 has increased and highlighted existing inequities for the hard-of-hearing in built and social environments. This affects the nearly one out of five people (1.5 billion people) who experienced hearing loss in 2019.
"What the hell are the deaf and hard-of-hearing supposed to do in a world where lips can no longer be read?"
Facial masks, an essential tool used to slow the spread of COVID-19, can decrease speech recognition for some people with hearing loss. They can obstruct facial expressions and lip movement, which are critical sources of non-verbal information. In a recent Hearing Health Foundation survey, a reported 85 percent of hearing-impaired individuals experienced difficulty reading lips covered by face masks during the pandemic. While clear face masks can reduce lip-reading challenges, access and usage can vary by setting, making it harder to navigate unfamiliar social contexts and communicate effectively.
Even accessing health care has become more difficult for hard-of-hearing individuals during the pandemic. Telemedicine platforms and hospitals with strict visitor restrictions do not always provide translation services for people with hearing loss. This was the case for Jenn Stringer, chief information officer at University of California, Berkeley, who is hard-of-hearing and was diagnosed with breast cancer in 2020. Due to COVID-19 restrictions, Stringer could not bring her husband into medical appointments to translate her medical advice.
"They always tell you to bring somebody in with a doctor when you're getting bad health news, right? Because you need somebody else to hear. And that was completely unavailable because of COVID," Stringer wrote about her experience.

Additionally, when hard-of-hearing people are hospitalized due to COVID-19, they experience distinct challenges such as difficulty adjusting hearing equipment or utilizing interpretive devices. This is compounded by the fact that over 60 percent of hearing-impaired individuals are older than 50 years, age groups that seek medical care at higher rates and are at greater risk of COVID-19 complications.
These communication challenges are not exclusive to adults. An estimated 70 million children with hearing loss are under the age of 15. Over the past year-and-a-half, many have experienced inaccessible remote schooling environments, limited interpretive services, and increased vulnerability to stress. Remote learning environments decreased access to speech sounds for many hard-of-hearing children, which affects spoken language and social development. Additional research is needed to characterize the long-term impact of remote learning and social distancing requirements on younger individuals with hearing loss.
The disparate impact of COVID-19 on vulnerable populations has produced a renewed focus on health equity. Many disability activists state that hearing loss is not an intrinsic deficit, but rather that disability is rooted in the conflict between functional capability and the social environment. The pandemic presents an opportunity to develop infrastructure that is more inclusive of deaf and hard-of-hearing populations, a historically overlooked group. While social distancing strategies are critical to slowing the spread of COVID-19, particularly with the rise of the Delta variant, it is also critical that inclusive policies such as clear face mask usage, closed captioning in telecommunications and speech-to-text applications are implemented to safeguard the well-being of vulnerable groups.
Remote learning environments decreased access to speech sounds for many hard-of-hearing children, which affects spoken language and social development
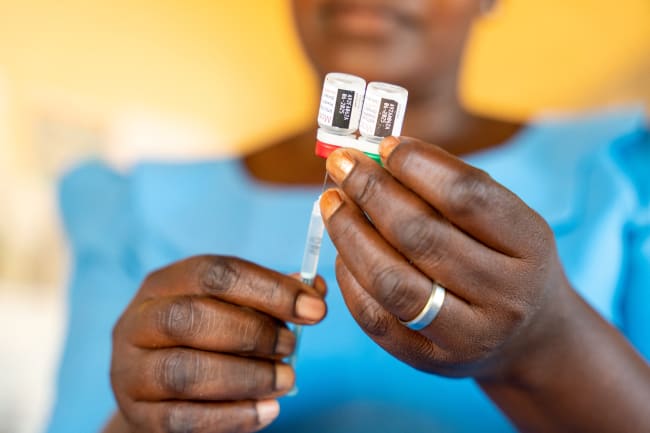
We must also realize that efforts need to be intersectional, with a focus on subpopulations at greatest risk of harm. Over 80 percent of people with moderate-to-complete hearing loss reside in low- and middle-income countries (LMICs). The hard-of-hearing in LMICs may endure extended periods of social distancing and prolonged communication challenges compared to people in high-income locations due to inequities in vaccine access. Challenges are compounded by limited access to hearing aids and other assistive devices. Globally, an estimated 83 percent of people in need of a hearing aid do not utilize one due to lack of access.
In the 2021 World Hearing Report, WHO Director-General Dr. Tedros Adhanom Ghebreyesus wrote, "As we have struggled to maintain social contact and remain connected to family, friends, and colleagues, we have relied on being able to hear them more than ever before."
But for people who have hearing loss, the challenge to be heard during this pandemic is greater than it is for those who can hear well. We can take common-sense measures to improve the well-being of people with hearing loss. Providers should be aware of the disparate impact of social distancing on hard-of-hearing people who communicate via spoken language. Accommodations should be widely available and encouraged to reduce barriers to communication and social support. Patients, providers, and people with hearing loss can refer to resources on effective communication, virtual learning, and accessible health care throughout the pandemic. As our pandemic environments continue to evolve, policy-makers must make accommodations to protect at-risk groups and achieve health equity.

EDITOR'S NOTE: The authors are employed by the University of Washington's Institute for Health Metrics and Evaluation (IHME), which leads the Global Burden of Disease study described in this article. IHME collaborates with the Council on Foreign Relations on Think Global Health. All statements and views expressed in this article are solely those of the individual authors and are not necessarily shared by their institution.