Late in 2021, San Francisco Mayor London Breed declared a state of emergency in the city's Tenderloin district to enable a quick and coordinated response to the opioid overdose crisis—driven mostly by fentanyl—that was killing more than two people a day.
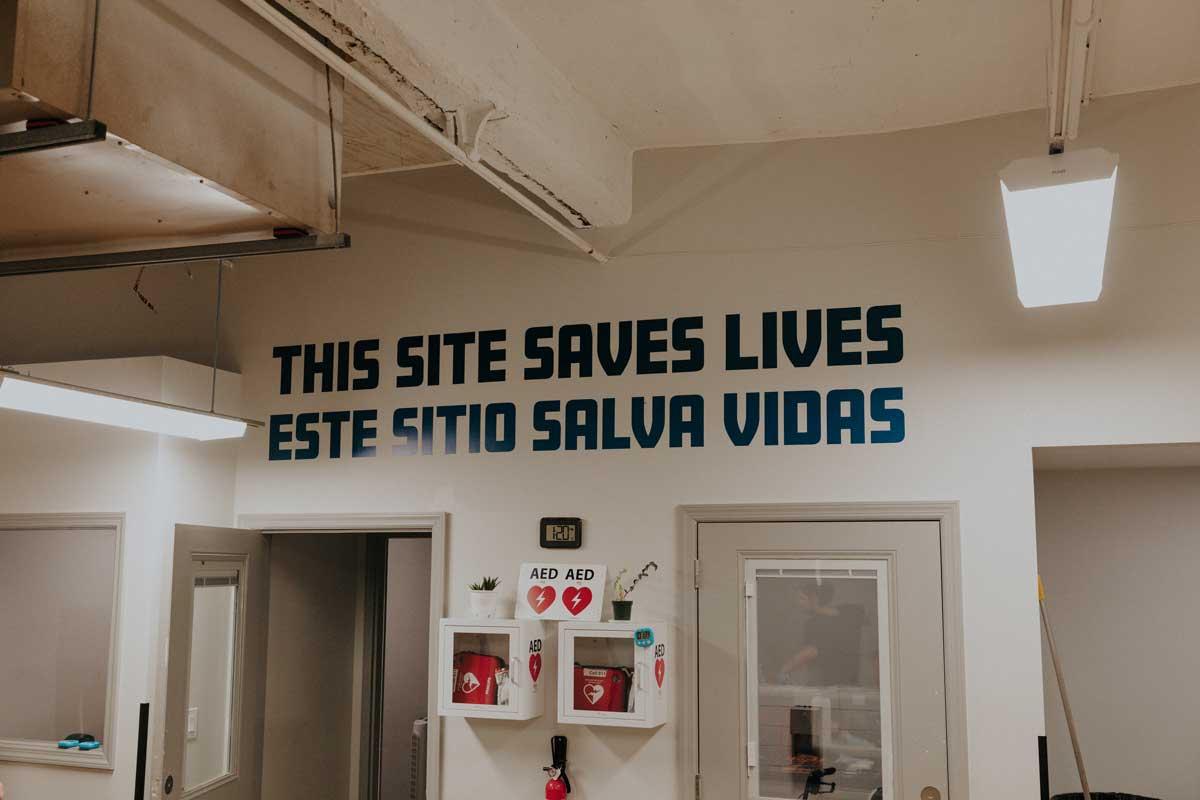
The Tenderloin Center opened in January 2022 and began offering behavioral health care, medical services, and other resources to people using drugs. Within a week, its scope covertly expanded to include an overdose prevention site (OPS). Also referred to as overdose prevention centers, supervised injection sites (SIS), and supervised consumption sites (SCS), these facilities give people a safe place to use drugs while they are monitored by staff trained to respond to an overdose.
"What was quickly realized was that there was nowhere to link people to, that evidence-based drug treatment slots were mostly at capacity," explained Alex Kral, an epidemiologist at the nonprofit research institute RTI International who led an independent evaluation of San Francisco's OPS. People were found using drugs in the Tenderloin Center bathrooms; the goal was to reduce their risk of harm as they waited for necessary care and services.
The drug treatment nonprofit running the Tenderloin Center—HealthRight 360—developed a welcoming community that accommodated up to 50 people. In addition to overdose prevention, it provided wraparound services to meet basic needs such as sterile supplies, food, showers, and laundry; clinical care, substance use disorder, and mental health treatment; and shelter placement, housing, and employment services. The OPS operated on the principle of radical hospitality and offered recreational activities from art to karaoke. About 300 to 400 people accessed the OPS daily to smoke or inject drugs, spending an average of 2.8 hours, a total of more than 18,000 hours a month.
"People wanted to be there," Kral said.
SF Mayoral Candidates Shift Focus From Harm Reduction
But the city's lack of transparency about the OPS, which operated outside the Tenderloin Center behind a covered chain-link fence, and its location in a heavily trafficked tourist area on Market Street near a BART (Bay Area Rapid Transit) station quickly raised public concern. The site closed in December 2022, despite evidence showing that it saved lives, including reversing 333 overdoses, and did not increase visible signs of drug use or homelessness in the neighborhood.
Accidental overdose data from San Francisco's Department of Health shows that deaths rose to 810 in 2023, up from 642 in 2021, 649 in 2022, and a previous record of 726 in 2020. As of August 31, preliminary data reported by the city shows that 412 people have overdosed in 2024.
Still, four of the five leading mayoral candidates for the November 4 election in San Francisco, including incumbent Mayor Breed, whose office declined multiple requests for comment, are running on a platform of more policing, less harm reduction—a backlash that Brandon Marshall, an epidemiology professor at Brown University, has seen in other areas including Oregon.
Many of these places are also experiencing severe housing crises
Brandon Marshall, epidemiologist, Brown University
"Many of these places are also experiencing severe housing crises, with unprecedented numbers of people unhoused or living on the street," he said. "But it's very easy to blame harm reduction programs or other progressive laws to address the overdose crisis for the increase in visible public drug use."
Public and political opposition to harm reduction is also evident in Vancouver, Canada, a city that has long endorsed this approach and opened the first supervised injection site in North America more than 20 years ago. Called Insite, it is one of three SCSs in Vancouver, of a total 39 in the country, that are authorized by Health Canada and currently operating in the city's Downtown Eastside (DTES) neighborhood. Like San Francisco's Tenderloin district, the DTES is at the center of Vancouver's—and more broadly Canada's—overdose crisis.
Against this backdrop, preliminary data recently released by the Centers for Disease Control and Prevention shows that U.S. overdose deaths have fallen for the first time since 2020, dropping about 10% to 101,168 for the year ending in April 2024.
Public health experts and researchers are attributing the decline to the increased availability of naloxone and medications for opioid use disorder. This trend is mirrored in British Columbia, where the BC Coroners Service reported a 9% decrease in overdose deaths (1,158 total) for the first six months of 2024 relative to 2023.

Politicians Still Ignore Robust Evidence Supporting Insite
When Insite opened in 2003, researchers pored over police reports and other available data to identify any unintended consequences.
"We found it was actually improving public disorder by taking people out of public environments where they were using drugs and into health-care facilities," said Thomas Kerr, a social medicine professor at the University of British Columbia, who led the initial evaluation of Insite.
Additional research showed that the neighborhood's fatal overdose rate decreased by 35% within two years and that frequent SIS users were 70% less likely to report syringe sharing. Other studies demonstrated that Insite's opening was associated with fewer ambulance calls, reduced incidence of HIV infections, increased initiation of addiction treatment, shorter hospital stays for injection-related skin infections, and decreased medical care costs.
Still, British Columbia Premier David Eby, who is in a tight race for a second term in the provincial elections being held October 19, is among the politicians shifting their approach to drug treatment. Last April, he ended a new drug decriminalization policy; in September, he proposed instituting involuntary treatment for people with serious addiction and mental health issues. Eby leads the leftist New Democratic Party in the province, where more than 14,000 people have fatally overdosed since a public health crisis was declared in 2016.
"We know that the current response that we offer is not adequate," Eby said at a September 15 news conference. "It is costly for people struggling with these conditions. They are not safe, and increasingly I'm concerned that the way they are interacting in our communities is making everybody less safe."
Although too few details were released to determine whether the province has capacity for both people forced into treatment and those who want to enter voluntarily, "there's a really good body of literature showing that involuntary treatment is not effective and can actually produce harm," Marshall said. This literature includes recent findings that an expansion of involuntary civil commitment in Massachusetts failed to meet its public health goals.
This is not just about harm reduction. It's about compassion and providing a pathway to recovery for those struggling with addiction
Gustavo Rivera, New York state senator
Nationally, Conservative Leader Pierre Poilievre is promising to defund harm reduction strategies, a plausible threat despite the unanimous Supreme Court of Canada ruling in 2011 that affirmed Insite's exemption from prosecution under federal drug laws. "During its eight years of operation, Insite has been proven to save lives with no discernible negative impact on the public safety and health objectives of Canada," the justices wrote.
"People are acting like this court case never happened, that there wasn't serious consideration of the evidence," said Kerr. Supervised consumption sites are "an area of drug policy that has been grossly politicized and that politicization has fueled the dissemination of misinformation. It's ignored science," he added.
U.S. OPCs Operating With Community Support
In the United States, currently two authorized overdose prevention centers are operating in New York City. Another is scheduled to open late this year in Providence, Rhode Island.
These sites were approved through distinct processes—New York City's OPCs by the mayor's office and the city's health department, and Providence's OPC the first to be authorized by state law and funded with opioid settlement dollars. (Minnesota and Vermont have also passed state legislation to establish OPCs.)
"New York City was able to open two overdose prevention centers through a combination of advocacy, community support and a public health approach," New York State Senator Gustavo Rivera, who chairs the body's health committee, wrote via email. "The most important factor, however, was the severe impact of the opioid crisis in NYC, which highlighted the importance of harm reduction in addressing substance use disorders as part of a broader public health strategy."
Similarly, in Providence, public and private harm reduction advocates spent years educating their communities about the goals of OPCs and the research supporting them. It's an approach that resonated in the close-knit state, where most people have a family member, friend, or colleague affected by the overdose crisis. "I've not seen a significant groundswell of antiharm reduction sentiment building here in Rhode Island," said Marshall, who is leading a National Institute on Drug Abuse–funded study of the New York City and Providence OPCs.
Early findings from the East Harlem and Washington Heights OPCs demonstrate that they have not increased crime or social disorder in New York City. Rivera, who is running for reelection, said the neighborhood stakeholders he meets with monthly in the Bronx, which has the highest overdose rate in the state, do not believe that criminalization is the solution. He plans to reintroduce the Safer Consumption Services Act in the next legislative session.
"This is not just about harm reduction. It's about compassion and providing a pathway to recovery for those struggling with addiction," Rivera wrote.