The world faces more armed conflict than at any point since World War II. One in six children live in or near a conflict zone. Armed conflict often blocks children's access to food, clean water, and health care.
A study in The Lancet on armed conflicts across the African continent found that infant deaths indirectly caused by armed conflict outnumbered all deaths from direct violence 3 to 1. Globally, more than 2 million children die each year in conflict-affected and fragile states, 48% of all under-5 child deaths.
As physicians who partner with communities hit by crisis and armed conflict, we have seen how the atrocities of war strike children disproportionately. Our consortium's new research from Mali, which ranks the 20 nations facing the most severe armed conflict, shows how rural communities reversed these deleterious effects. Published on September 1 in the Bulletin of the World Health Organization, the study shows when children were able to access locally led health-care services quickly, their chances of surviving conflict increased dramatically.
The trial, a partnership between researchers at the University of Bamako, the University of California in San Francisco, the University of Michigan, the London School of Hygiene and Tropical Medicine, the Malian Ministry of Health, and the nonprofit Muso followed 135,149 people in Bankass, Mali, from 2017 through 2020.
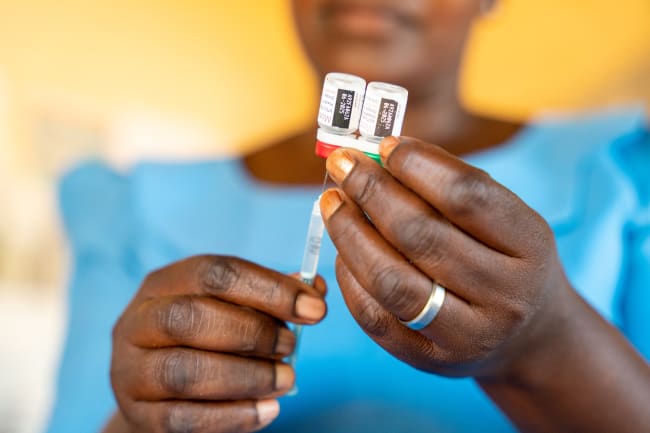
It began during peacetime and sought to measure the effectiveness of one medicine's oldest institutions—the house call—relative to visiting a health worker working from a fixed site in the village. The study both provided free health care from community health workers in each village and upgraded public clinics.
Although the trial did not intend to study child survival during armed conflict, the conflict spread into the area, escalating into massacres and the burning of villages.

One would have expected infant and child death rates to rise as conflict violence erupted relative to the pre-study period. The opposite happened. Despite the surrounding armed conflict, mortality among children younger than 5 plummeted by 63% over the three years preceding the trial. Children were far more likely to survive than they were in peacetime without enough access to timely health care.
Half of the communities were randomly selected to receive care from a community health worker through door-to-door house calls. The other half received care from community health workers who stayed at a fixed-village site and did not make house calls. Nearly all health-care providers came from and lived in the areas they served.
The home visits improved preventive care: Pregnant women got earlier and more complete prenatal care. Parents sought care for their children faster and more frequently even amid the conflict than before the study period. Improvements in child survival, regardless of whether families got a house call, were comparable in both groups.
Those results suggest that access to free quality health care close to home could help reverse the damage of armed conflicts on under-5 child mortality. Every conflict and context is different, and results from one setting do not automatically apply to another. Yet fees and long distance can impede access to care during peacetime and more so in conflict. When leaving one's home involves danger, and violence can rob families of their assets, health care can be designed to overcome these barriers.
When leaving one's home involves danger, and violence can rob families of their assets, health care can be designed to overcome these barriers
Amid the spread of armed conflict, 59 nations are not on track to meet the Sustainable Development Goal for child survival by 2030. These trial results, however, show that it is possible to accelerate progress on child survival even in the midst of armed conflict.
Members of the public can contribute to health care that supports local providers and removes fees for patients, and urge their representatives to do the same. Governments, foundations, nonprofits, and financing institutions can prioritize and increase contributions to resilient local health care and child survival in conflict settings. Only 1% of the U.S. 2023 budget went to foreign assistance, of which only 9% was committed to supporting children. Other research suggests that investments in health care may also increase stability and reduce violence.
The achievements of the communities in this trial may be unprecedented but should not remain outliers. Beyond short-term humanitarian relief, accessible health care without fees could drive enduring improvements in health outcomes, even during armed conflict.
Such locally led health care merits far more investment, particularly for children in conflict zones. It is time to reimagine what is possible in the midst of armed conflict and to commit accordingly.