The COVID-19 pandemic has now sparked a secondary pandemic of vaccine nationalism. Around the world, countries are "going it alone" to make bilateral vaccine deals, threaten intellectual property protections, and generally use whatever means necessary to secure access for their citizens. This is an understandable political response—perhaps—but one whose ultimate outcomes are likely to be suboptimal and inequitable, even for the largest and wealthiest countries like the United States.
A risk that much of the world will be left behind—countries not funding their own vaccines, with no specialist manufacturing, and lacking buying power
The current unilateral scramble for vaccines creates a number of risks. First, countries are betting on their "own" national vaccine candidates—but what if those candidates are unsuccessful? By putting all their eggs in one or two baskets, countries increase their own exposure to failure risk. And when countries fail to cooperate, the effective global "portfolio" may itself be unbalanced and suboptimal, increasing the risk that no vaccines succeed. Countries may end up "paying twice" for vaccines by using "push" funding, i.e. subsidising research and development (R&D) up front and then paying vaccine prices that do not account for public investment and/or exceed the health benefits delivered. Furthermore, significant public funding to advance a subset of candidates may crowd out private investment in other candidates undermining the healthy pipeline needed to provide second- and third-generation vaccines. Threats to seize intellectual property will further dissuade at-risk private investment. And most importantly, there is a risk that much of the world will be left behind: most countries are not funding their own vaccine candidates, have no specialist manufacturing capability, and lack the buying power to get to the front of the purchasing queue on their own.

An appropriate global response should balance development risk between countries, ensure access at cost to low- and lower–middle- income countries, incentivize private investment in vaccine R&D, and engage the "missing middle" of middle-income countries and the higher income countries without national candidates. Regional or global coordination will also send clearer demand signals to developers. And as we have previously argued, implementing "pull" incentives (adding purchasing power) is essential to drive private investment and ensure a health pipeline of candidates, complementing existing push funding for R&D and manufacturing.
To drive R&D for vaccines against COVID-19
Specifically, we've proposed a new pull mechanism—the benefit-based advance market commitment—designed to drive R&D for vaccines against COVID-19. We believe the principles of this approach can substantially increase the effectiveness of the two most prominent global and regional initiatives, respectively the Gavi COVAX Facility and the EU Joint Procurement Proposal.

Existing Cooperation Mechanisms: What's in the Scope?
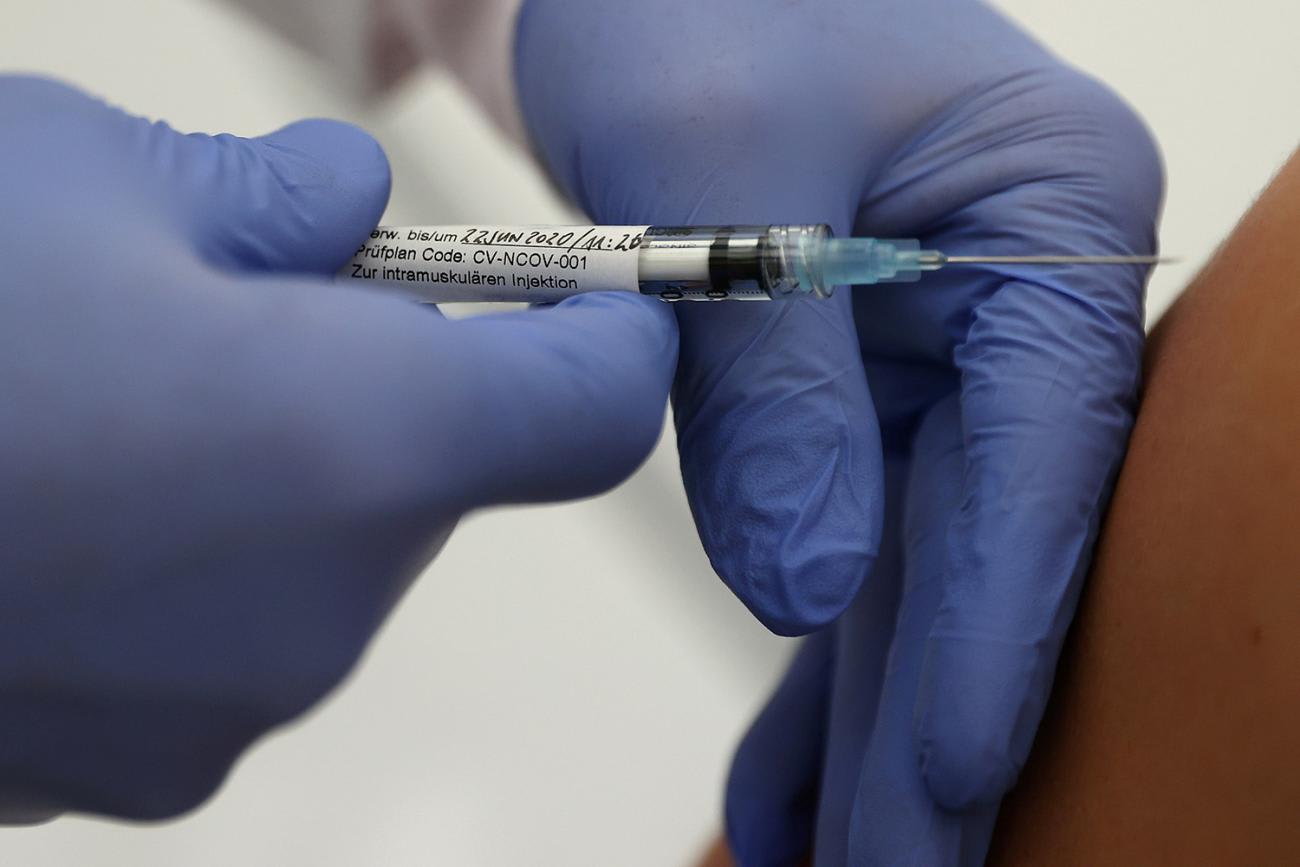
The Gavi COVAX Facility was launched in June as part of the WHO vaccine pillar. It is intended to add buying power to complement investments by the Coalition for Epidemic Preparedness (CEPI) in R&D and manufacturing capacity for vaccine candidates. It involves two types of pull mechanisms to procure vaccines. Firstly, volume guarantees to specific manufacturers, contingent on them meeting the agreed WHO target product profile. This requires "overbuying" as no-one knows how many vaccines will be successful. Secondly, a market-wide demand guarantee. Here there is no overbuying, the guarantee is purchase an overall quantity. Developers take the risk as to whether countries choose their vaccines. The COVAX Facility intends to support a continued pipeline of improved products coming to market. The current emphasis—and operational detail—is placed on the short term "manufacturer-specific volume guarantee," rather than the longer-term "market-wide demand guarantee."
It's not yet clear how many expressions of interest will translate into legally binding pledges or disbursements
So how will it work? The details are not yet finalized. Drawing on Gavi's existing approaches and limited public communications, we anticipate that the facility will solicit expressions of interest from manufacturers to supply vaccines at pre-set prices and volumes. Gavi, in turn, will make legally binding commitments to purchase from specific manufacturers. These agreements would be backed by purchase commitments from two major vaccine buyers, The United Nations Children's Fund (UNICEF), and the Pan American Health Organization (PAHO), and individual "self-financing" countries. The financing structure, legal agreements and governance mechanism are still in development. While tens of non-donor-backed countries have expressed an interest, it is not yet clear how many will translate into legally binding pledges or disbursements.

Importantly, the facility stops short of creating a market based on its portfolio of country commitments. Instead, it proposes a series of volume commitments to individual manufacturers for specific products, which will be triggered if and when they receive a license, and may result in too much or too little delivered vaccine.
The EU has proposed using its joint procurement powers to secure vaccine doses for its twenty-seven member states
The European Union has a regional mechanism for cooperation. It has proposed using its joint procurement powers to secure vaccine doses for its twenty-seven member states. Advance purchase agreements with vaccine producers will secure the right to buy a specified number of doses at a given price (as in the COVAX manufacturer-specific volume guarantees). In some cases, the European Union will secure this right by partially funding developers' upfront costs. Early engagement between the European Medicines Agency (EMA)—Europe's FDA equivalent—and manufacturers is already underway. An EMA license will be the sole quality and performance hurdle for procurement.
A Different Approach to Sharing Risk
Under the current Gavi and European Union approaches, countries and donors subsidize development risk through large upfront push commitments or advance purchase agreements. These arrangements may lock countries into purchasing vaccines that meet regulatory requirements—even if those vaccines are ultimately less appropriate or effective than other potential options.
We propose a different approach to risk sharing, where the private sector retains most R&D risk and countries only pay for a successful vaccine
We propose a different approach to risk sharing, where the private sector retains most R&D risk and countries only pay for a successful vaccine. Countries assume market risk by guaranteeing an overall market for COVID-19 vaccines, even if the need for those vaccines decreases unexpectedly in future years (making such expenditure otherwise unnecessary). This is close to the COVAX longer-term "market-wide demand guarantee." Our proposed benefit-based advance market commitment is adapted from an earlier proposal for bringing to market new tuberculosis drugs, which in turn is an adaptation of the pneumococcal vaccine advance market commitment successfully implemented by Gavi to the benefit of —but with two important differences. First, the new approach uses value-based pricing across multiple purchasers (resulting in country-specific tiered pricing) rather than a single, uniform price for a single global or regional purchaser. Second, our approach is large enough to stimulate R&D and manufacturing capacity investment.
A benefit-based advance market commitment (BBAMC) for a COVID-19 vaccine would work in a stepwise fashion. First, early health technology assessments by a country—or a regional or global purchaser acting on their behalf—would establish a value-based price for a product meeting the WHO target product profile. It would ensure risk sharing with payers, as the early health technology assessment is used to identify the size of each country's advance commitment based on the volume of vaccine needed and the price per dose.
Our proposal would enable delivery of manufactured vaccines around the world, including to the poorest nations
This market value would be "locked in" in advance, contingent on meeting the minimum target profile, to provide overall market predictability to manufacturers. In the second step, our proposed scheme would aggregate these individual country commitments. These value based market commitments must be guaranteed by a credible third party (such as the World Bank, regional development banks and/or independent national central banks) and offered (with country-specific tiered prices) to developers that meet the minimum WHO target profile. Such guarantees would help maintain interest from potential innovators after a first vaccine is launched, hedging risk against late failure or safety risks from one or more early candidates/entrants. In the final step, our proposal would enable delivery of manufactured vaccines around the world, including to the poorest nations. How would this work? To access the purchase commitment, the successful innovator must agree that volumes beyond the guaranteed advanced commitments will be sold at a lower "tail" price, close to manufacturing cost, equivalent to the price of a generic drug after patent expiry. Low-income countries would be supplied from the start at this tail price. Successful innovators could license their vaccines and manufacturing processes out to other suppliers or local licensees in order to facilitate widespread availability to the poorest countries at a low price.

Effective governance arrangements would be needed. We offer a general discussion and options analysis in our value based advance market commitment proposal for a TB cure. The governance arrangements will need to include allocation rules between participating countries that override pricing considerations (e.g., higher-tiered prices in some countries than others).
Manufacturers are not required to participate in the mechanisms, but if they choose to join, they must agree to make certain quantities available to participating countries, directly or by agreeing to licence their products and technologies to other manufacturers. There is no commitment on the part of participating countries to buy any particular vaccine—only to buy qualifying vaccines over a time period to meet the total market value commitment.
What the Benefit-Based Advanced Market Commitment Looks Like
Comparing elements of the COVAX/EU joint action proposals with the authors' own vaccines proposal
Merging COVAX and EU Joint Action with a Benefits-Based Advance Market Commitment
If manufacturers and governments and international funders are already "locked" into push funding and contingent advance purchasing agreements, it may be too late to radically change the buying mechanism—at least for the current leading vaccine candidates. Even so, it may be feasible to both introduce a benefits-based advance market commitment for a second wave of candidates, (or for future emergent pathogens) and to incrementally improve existing mechanisms by adding elements of the latter to existing deals.
Specifically, there are three ways in which the COVAX Facility and the EU Joint Action could be improved to incorporate key elements of a benefits based advance marker commitment.
It may be too late to radically change the buying mechanism—at least for the current leading vaccine candidates
First, current arrangements must reward vaccine value through affordable value-based prices rather than cost-based or arbitrary prices. To avoid getting locked into purchasing low-efficacy vaccines, deals with manufacturers should incorporate value assessment based on each country's ability to pay. At a minimum, the deal is only valid at the agreed value-based price if the vaccine meets WHO target product characteristics based on modeling against epidemiological, health system delivery, and demographic characteristics. The total payment (market value) for vaccines could also scale up progressively with vaccine effectiveness, with differential prices across countries reflecting local benefit and ability to pay. (See detailed technical discussion on pages 28-31 here [PDF]).

Second, both Gavi and the European Union ought to ensure benefits exceed costs before rollout through at-launch health technology assessment as is the norm for most new high value products in developed markets. Countries may be tempted to roll out low-efficacy vaccines because of the sunk cost fallacy ("we paid for them, so we may as well use them") even though the costs of rollout exceed the benefits. We need to ensure that use of a vaccine in any patient group generates net benefits, especially given vaccine hesitancy and breakdowns in trust between the scientific community and general population. Use of Health Technology Assessment (HTA) before rollout—even if the vaccine price is a sunk cost—can help ensure accountability and due process, plus offer a structured process to course correct as new information emerges. Such assessments would not affect vaccine prices or committed volumes (assuming products reach the minimum performance threshold).
A market-wide commitment could also increasing private sector investment in other promising candidates
Third, current and currently negotiated deals must move from one-off bilateral "deals" to true market commitments. Market-wide advance purchase commitments tied to value, versus one-off deals for specific candidates, can help countries avoid lock-in to purchasing low-efficacy vaccines even if better vaccines become available. A market-wide commitment could also increasing private sector investment in other promising candidates, the overall probability of successful vaccine development, and some degree of private investment in manufacturing scale. However, at-risk manufacturing scale-up to serve low- income countries may still require push funding by development partners and wealthier governments using aid monies.

Rapid pursuit by governments of vaccine development to protect their citizens is welcome. Let's hope that early candidates will generate evidence they deliver substantial health benefit. The reality is, however, that we are unlikely to find one "knock out" vaccine and a number will be needed. The procurement mechanism we propose will impact positively on the mobilization of private investment, on the quality of the vaccines that are developed, and on the speed with which they are made available to the world's poorest citizens.












