The COVID-19 pandemic underscored the importance of quickly identifying and responding to outbreaks before they reach epidemic levels. Crucial to that process is the timely reporting of outbreaks.
Although individual state policies and legal frameworks direct outbreak reporting from the local to the national level, the International Health Regulations (IHR) direct reporting of public health emergencies of international concern (PHEICs) by World Health Organization (WHO) member states and define core capacity requirements for states to detect such events. Under the current IHR (adopted in 2005), member states are required to report high-consequence public health events to the WHO within 24 hours of detection.
In the wake of COVID-19, WHO member states have begun negotiating reforms to the IHR and a separate agreement on pandemic preparedness and response. Many of the proposed reforms focus on improving states' technical capacity to detect high-consequence public health events and facilitating their reporting to the international community.
The proposed IHR reforms and pandemic agreement, however, do not address important political, economic, and social barriers to timely outbreak reporting from the local level to the national level. These barriers can worsen the course of a disease outbreak and present a formidable challenge to pandemic prevention efforts.
Member states are required to report high-consequence public health events to the WHO within 24 hours of detection
Advancements in Global Health Governance
In 2022, reforms began with the convening of both a working group to coordinate proposed amendments to the IHR and an intergovernmental negotiating body to develop a new pandemic agreement. If negotiations stay on track, member states are due to consider the two instruments at the seventy-seventh World Health Assembly in May 2024.
Many of the proposed reforms in the most recent drafts address two major barriers to outbreak reporting: weak surveillance capacity and fear of travel or trade restrictions.
Lack of appropriate surveillance capacity is an ongoing risk to global health security. In West Africa, for example, that deficiency delayed detection and reporting of an emerging Ebola outbreak in Guinea that subsequently grew into a multiyear epidemic. As a result, proposed amendments to Annex 1 of the IHR, which lists member state core capacity requirements, would expand the required capacities for the detection, assessment, and reporting of public health events at the local, intermediate, and national levels, including adequate surveillance and laboratory infrastructure.
In addition, an amendment to Article 54 would establish an Implementation and Compliance Committee to facilitate and oversee member states' progress toward meeting IHR requirements. Article 4 emphasizes member states' obligations to develop appropriate multisectoral surveillance capacities and to cooperate on their strengthening.

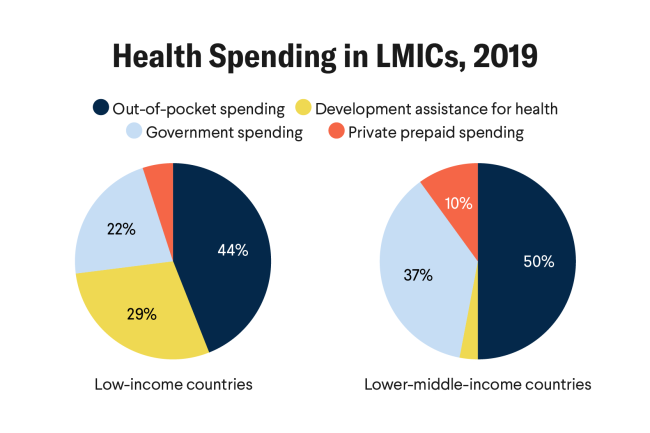
To meet those obligations, proposed amendments to Article 44 of the IHR codify the responsibilities of member states to financially assist each other, particularly developing countries, to implement the IHR, including identifying and reporting public health events. Mirroring the proposed IHR amendments, Article 20 calls for sustainable financing for pandemic prevention, preparedness, and response, including the establishment of a coordinating financial mechanism to complement the Pandemic Fund hosted by the World Bank. It remains unclear, however, how future mechanisms will ultimately be financed, questioning the success of such an initiative.
Economic Deterrents
The fear of damaging cross-border restrictions in the wake of reporting an outbreak is another significant reporting barrier. Under the current IHR, member states must not implement overly restrictive trade or travel measures given available alternatives and must justify to the WHO any significant travel or trade restrictions in response to a reported outbreak.
However, that process has done little to stop nations from imposing economically damaging restrictions during previous outbreaks. Several countries experienced substantial economic damage from travel or trade restrictions during the 2009 H1N1 influenza pandemic and 2014 Ebola epidemic, and South Africa experienced immediate travel restrictions after reporting a new SARS-CoV-2 variant during the COVID-19 pandemic.
Those consequences suggest that countries could be less likely to report an outbreak if they fear economic damage from such restrictions.
Movement Restrictions
To alleviate concerns that travel or trade restrictions could harm countries' reporting future outbreaks, a proposed amendment to Article 18 of the IHR stipulates that the WHO should account for the need to facilitate international travel, as appropriate, and maintain international supply chains in making recommendations affecting international traffic, particularly to ensure the free transit of health workers, health products, and food supplies to outbreak-affected areas. In addition, a proposed amendment to Article 43 requires that countries take measures to facilitate access to health products when implementing additional health measures.
A proposed amendment to the IHR stipulates that the WHO needs to account for the need to facilitate international travel
Those amendments attempt to strike a balance between the need to slow or prevent the international spread of an outbreak through travel and the need to ensure that affected countries are not physically and economically isolated from the world and have access to crucial outbreak response resources.
A state's means and will to detect and report outbreaks are viewed as the primary determinants of whether it reports an outbreak in line with IHR obligations, and the proposed global health governance reforms reflect this understanding. However, outbreak reporting relies on an uninterrupted flow of information from the local level to the national level, and political, economic, and social considerations could interrupt that flow at any point.
Neither the proposed IHR amendments nor the pandemic agreement address such nontechnical reporting barriers. Furthermore, any treaty or regulation that directs a country to reform deeply rooted internal social, political, and bureaucratic norms and behaviors would likely fail given concerns for national sovereignty. The following examples underscore both the variety and importance of such local reporting barriers across different settings.
Nontechnical Barriers to Outbreak Reporting at the Local Level Are Diverse and Global
The outbreak reporting process often begins with health-care practitioners and farmers, who are expected (and often legally obligated) to report suspected outbreaks. Despite those expectations, health-care providers and farmers might not be willing to report an outbreak for a host of reasons, including reputational harm. A 2016 study found hospital managers in Brazil reportedly suppressed clinician reporting of nosocomial outbreaks (outbreaks that begin in a hospital), potentially to avoid damaging their hospitals' reputations. Farmers in the Netherlands were reluctant to report notifiable animal diseases out of fear of being blamed for outbreaks on their farms.
Failure to report such outbreaks could delay detection and response to a new outbreak, including an emerging zoonotic pathogen. Although reputational concerns can prevent timely outbreak reporting at the ground level, officials between local actors and the national government can be motivated by economic and political concerns to suppress reporting of new outbreaks, such as fears of disrupting travel or important national events, the results of which can damage their careers, especially if the outbreak reports prove unfounded.
Indeed, those concerns were some of the most critical elements in shaping the initial outbreak response during the Severe Acute Respiratory Syndrome (SARS) and COVID-19 pandemics. In the early stages of these outbreaks, local officials downplayed their severity likely to avoid negative economic repercussions and disrupting important political meetings. The inaccurate flow of outbreak information to China's central government delayed the country's ability to fully recognize the severity of those outbreaks and mobilize an appropriate response.

Preventing the next pandemic requires a better understanding of the various nontechnical barriers and enablers of outbreak reporting at the local level.
The described barriers to outbreak reporting are not unique to specific countries but present worldwide. The WHO cannot reform a state's inner workings or propose options relevant to every national setting. Accordingly, an amended IHR or pandemic agreement also cannot remedy those barriers. Nevertheless, successful future pandemic prevention will in part hinge on successfully addressing them.
Although nontechnical barriers to outbreak reporting at the local level remain largely unexplored, the global health community can educate those responsible for outbreak reporting about the importance of timely and transparent reporting. Organizations such as the WHO, the Food and Agriculture Organization, the World Organization for Animal Health, and the United Nations Environment Program can develop learning modules to educate farmers, veterinarians, and health-care practitioners across a variety of settings on the importance of timely reporting and what and when to report, including events affecting people, animals, plants, and the environment.
Such interventions can leverage existing solutions to encourage reporting and explore novel ones to help build a multisectoral culture of reporting at the ground level, which is where outbreak reporting ultimately begins. Given the importance of local barriers to outbreak reporting during previous pandemics, efforts to normalize reporting at the local level will help prevent the next major outbreak from becoming another devastating pandemic.