President Donald Trump issued an executive order directing the United States to withdraw from the World Health Organization (WHO) in January. That decision marks a pivotal moment in global health governance and creates a leadership vacuum that threatens to disrupt progress in health-care equity, biosecurity, and capacity-building. Although medical accrediting organizations cannot fully replace the WHO's financial and mobilization capabilities, they can mitigate some of the risks posed by the withdrawal by leveraging their expertise to provide technical support, strengthen health-care systems, and foster collaboration.
Their efforts, however, should be part of a broader, collaborative approach that includes governments, multilateral agencies including the WHO, and private-sector stakeholders. The challenges associated with replacing the lost human and financial capital are immense, but so are the opportunities to rethink and strengthen the frameworks that underpin global health.
In this vacuum of U.S. leadership, medical accrediting organizations have a unique opportunity to assume a more significant role in sustaining global health progress. Organizations, including the Joint Commission International (JCI), Accreditation Canada, and the Australian Council on Healthcare Standards International (ACHSI), are well positioned to step up. With decades of experience setting and enforcing health-care quality standards, these entities can help fill gaps left by diminished WHO funding and leadership.
To navigate the complex geopolitical dynamics, however, these organizations should leverage their global reach, foster collaborations with regional and national bodies, and ensure that their standards remain neutral and flexible enough to address the diverse health priorities across different countries. Accrediting organizations should proactively engage with stakeholders, balance varying political interests, and demonstrate their value in fostering sustainable, equitable health-care systems that transcend borders.
The Risks of a Weakened WHO
Trump's executive order cites dissatisfaction with the WHO's handling of the COVID-19 pandemic and financial imbalances in member contributions, halts U.S. funding to the organization, and initiates the formal year-long withdrawal process stipulated by a 1948 Joint Resolution of Congress. The order also mandates reassigning U.S. personnel working with the organization.
The U.S. withdrawal will hinder disease surveillance efforts, making these systems less effective and increasing the risk of delayed responses
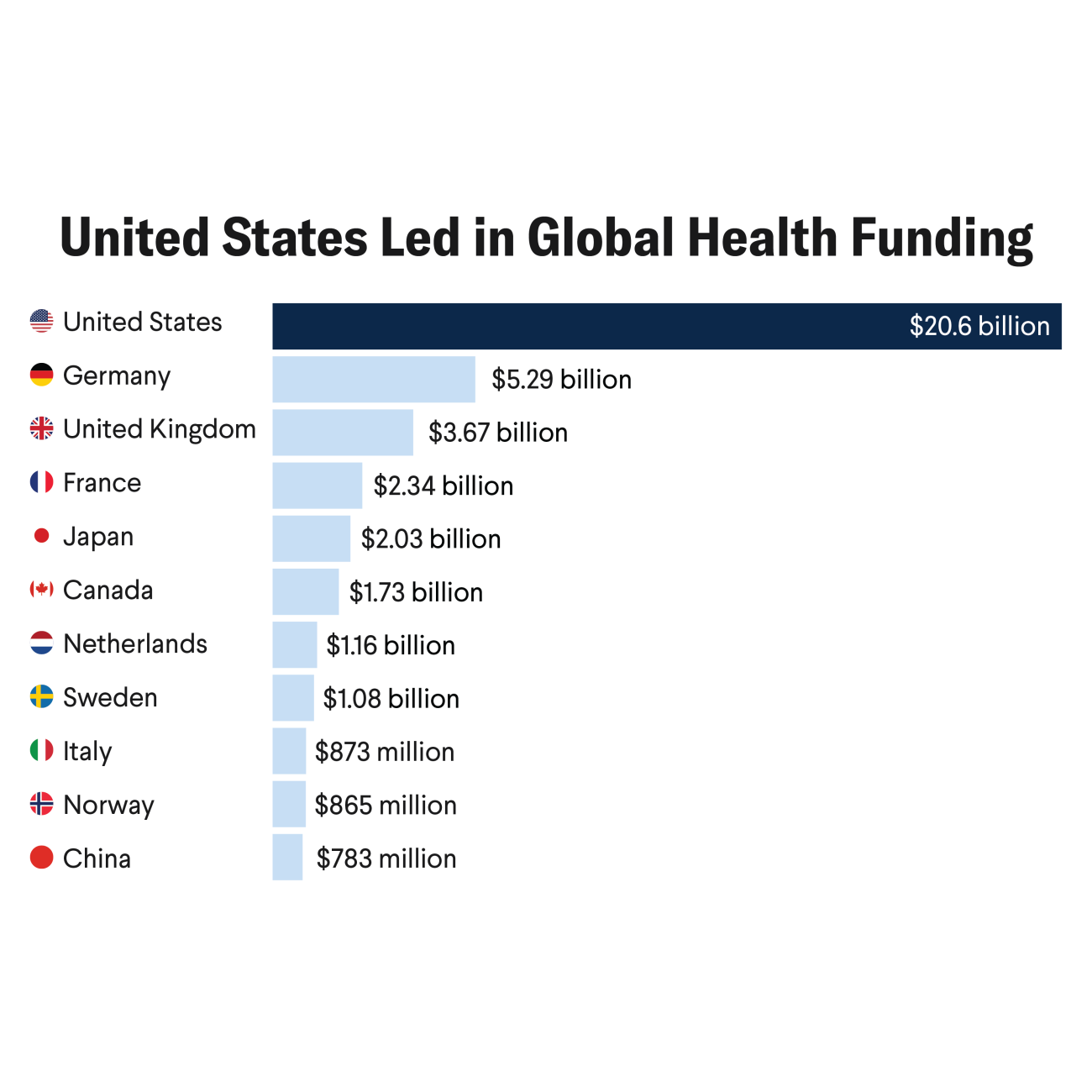
For decades, the United States has been the most significant single contributor to the WHO, providing up to $1.284 billion annually (2022–23) to fund programs that combat infectious diseases, improve maternal and child health, and build health systems in low- or middle-income countries (LMICs). The cessation of U.S. financial support threatens to disrupt those critical initiatives, jeopardizing progress in polio eradication, vaccination campaigns, and pandemic preparedness.
The decision will disproportionately harm LMICs, which rely heavily on WHO programs for technical assistance, funding, and capacity-building. Those countries could see setbacks in achieving the UN Sustainable Development Goals related to health, including reductions in maternal and child mortality and eradicating preventable diseases. The withdrawal threatens to widen existing health inequities, leaving millions of vulnerable people without access to essential services.
The Role of Medical Accrediting Organizations
Medical accrediting organizations are crucial in strengthening health-care systems by promoting best practices, reducing medical errors and fostering continuous improvement. Expanding their services to LMICs, particularly those affected by the loss of WHO support, could contribute to stabilizing and enhancing health-care delivery. The JCI collaborates with global health organizations and governments to improve health-care quality and safety worldwide. Through strategic alliances, such as partnerships with the National Association for Healthcare Quality, JCI supports efforts to enhance patient safety and health-care outcomes, which may benefit resource-constrained facilities in underserved regions.
Another area where accrediting organizations can make a difference is global health security. The WHO's global networks for disease surveillance, vaccine distribution, and emergency response are integral to preventing and mitigating pandemics, as seen during the COVID-19 pandemic. The U.S. withdrawal will hinder disease surveillance efforts, making these systems less effective and increasing the risk of delayed responses to emerging health threats. In the past, the United States has led efforts in monitoring, researching, and responding to public health threats, such as the 2009 H1N1 influenza pandemic, the 2014 Ebola outbreak, and the COVID-19 pandemic.
Accrediting organizations are pivotal in enhancing infection prevention, control, and emergency preparedness within health-care systems. For instance, the JCI's rigorous accreditation standards have been shown to improve infection control measures in long-term care hospitals.
Similarly, Accreditation Canada offers comprehensive infection prevention and control programs that provide evidence-based standards and guidelines to health-care facilities. These programs are designed to help organizations implement the best infection prevention and control practices. By providing such accreditation programs, these organizations ensure that health-care facilities adhere to high infection prevention and control standards, enhancing their capacity to manage health crises effectively.
Medical accrediting organizations can also play a vital role in fostering collaboration. Without U.S. leadership, the global health community will face a vacuum in the transparency and accountability that it often championed. Further, China could use this void to broaden its Health Silk Road initiative to include critical health-care infrastructure and medical expertise. As neutral entities, medical accrediting organizations are well suited to convene governments, nongovernmental organizations (NGOs), private-sector stakeholders, and academic institutions.
Accrediting organizations are pivotal in enhancing infection prevention, control, and emergency preparedness within health-care systems
The JCI, which partners with governments and health-care providers worldwide to establish global standards for health-care quality and patient safety, is one example. Its collaborations include working with Saudi Arabia to enhance health-care quality and its partnerships with global organizations such as the WHO to integrate best practices in infection control and clinical outcomes measurement. These partnerships have helped improve health-care systems in countries with varying levels of infrastructure, resulting in more transparent, accountable, and effective health-care services. Such collaborations can amplify the impact of health initiatives, ensuring that resources are used efficiently to address complex challenges. This model of cooperation could serve as a guide for sustaining global health progress after the U.S. withdrawal.
These examples suggest pathways for accrediting organizations to amplify their impact. By collaborating with multilateral donors, NGOs, and philanthropic foundations, they could secure the resources needed to expand their operations. They could also explore new funding models, such as blended finance or public-private partnerships, to enhance their financial sustainability and reach.
Challenges and Opportunities
Despite their potential, accrediting organizations face significant challenges. Expanding their reach to underserved regions requires substantial financial and human resources. Accrediting organizations are not equipped to replace U.S. financial contributions or the ability to mobilize countries. Although they can provide technical assistance and capacity-building, they do not have the infrastructure or funding mechanisms to fill the funding gap left by the United States or to coordinate large-scale health initiatives.
This limitation underscores the need for broader partnerships and innovative solutions to address the void left by the U.S. withdrawal. Another hurdle is building trust and overcoming resistance in local contexts, where accreditation could be considered an external imposition, particularly in LMICs, where resources are scarce and health-care priorities differ from those of high-income countries. Additionally, navigating geopolitical dynamics while maintaining neutrality will be essential to preserving their credibility.
Accrediting organizations should adopt strategic approaches to overcome these obstacles. Partnerships with global health donors, private philanthropies, and technology companies could provide the funding and technical expertise needed to scale operations. Building strong local partnerships and adapting accreditation programs to fit cultural and contextual realities will be key to gaining acceptance and ensuring sustainability. Embracing innovation—such as telemedicine, data analytics, and tele-accreditation—can enhance their ability to deliver services efficiently and widely while monitoring real-time progress.
The U.S. withdrawal from the WHO is a critical turning point in global health governance, creating a leadership gap that medical accrediting organizations are uniquely positioned to help fill. Although these organizations cannot replace the extensive resources or financial support the WHO provides, they can play a pivotal role in stabilizing and enhancing health-care systems, particularly in LMICs.
Through collaboration, adaptation, and leveraging their expertise, accrediting bodies such as the JCI, Accreditation Canada, and the ACHSI can mitigate the risks associated with the U.S. withdrawal. A holistic approach that involves multisector partnerships, innovative funding models, and local contextual adaptation will be essential to ensuring sustainable and equitable global health progress. Despite the challenges, this moment also presents an opportunity to rethink and reinforce the frameworks that underpin global health, creating a more resilient, collaborative, and adaptable global health infrastructure for the future.