Lenacapavir (LEN), a groundbreaking HIV-1 capsid inhibitor developed by Gilead Sciences, stands on the brink of revolutionizing HIV prevention. As a potential long-acting pre-exposure prophylaxis (PrEP) option, it could transform the fight against the epidemic. Yet uncertainty surrounds its future pricing and accessibility, raising urgent questions for the communities hardest hit by HIV.
"Revolutionary innovations lose their impact if they remain out of reach for those who need them most," emphasizes Danielle Campbell, a science equity activist, founding member of PrEP in Black America, and member of the Gilead Sciences Community Accountability Group. Her sentiment echoes a broader challenge that continues to plague the global HIV response: the delicate balancing act of innovation and equitable access.
In June 2024, Gilead Sciences unveiled encouraging results from its Phase III PURPOSE 1 trial (NCT04994509) for lenacapavir, which demonstrated that the treatment prevented 100% of HIV acquisition in cisgender women. A subsequent Phase III PURPOSE 2 trial (NCT04925752) reported a 96% prevention rate across diverse groups—including cisgender men, transgender men, transgender women, and gender nonbinary individuals who have sex with men across seven countries, including the United States.
Revolutionary innovations lose their impact if they remain out of reach for those who need them most
Danielle Campbell, PrEP in Black America
This week, the fifth HIV Research for Prevention (R4P) Conference is taking place in Lima, Peru, where policymakers, researchers, advocates, and civil society stakeholders are convening to discuss the challenging and fast-growing field of HIV prevention research. To ensure the successful and equitable introduction of lenacapavir, we recommend a comprehensive, multipronged 4P strategy centered on equity:
Participation: Intentional and proactive community engagement and mobilization to address and dismantle structural barriers. For example, during the West Africa Ebola Outbreak (2014-2016), large-scale, structured community engagement was critical for epidemic control.
Policy: Mobilize political will and advocacy toward President's Emergency Plan for AIDS Relief (PEPFAR), the Global Fund, and other donors to negotiate pricing and volume guarantees with Gilead, securing a sustainable supply during lenacapavir's initial introduction period and until generics become available.
Parallel implementation: Funders, ministries of health, implementers, and civil society should design an introduction strategy that breaks away from traditional sequential approaches. By moving toward a parallel process—simultaneously preparing regulatory submissions, scaling up manufacturing, planning distribution channels, and integrating with health systems—access to both branded and generic versions can be accelerated and potentially fast-tracked.
Pricing: Affordable pricing is crucial. Using cabotegravir pricing models as a benchmark presents inherent challenges because the drug is already prohibitively expensive for many markets. Advocates should push for full transparency from Gilead Sciences, urging that lenacapavir not only be priced competitively with cabotegravir but also actively seek ways to undercut it, driving the price toward the level of generic oral PrEP as quickly as possible.
Paying for a New Era of HIV Prevention
Amid the celebration over lenacapavir, a familiar concern looms: affordability.
The treatment version of lenacapavir, branded Sunlenca, comes with an annual price tag of $42,250. Looking at the current U.S. market for HIV prevention, Gilead's earlier PrEP medications, Truvada (generic versions available for $300 per year) and Descovy (daily oral pills) cost more than $21,000 per year, and cabotegravir (another long-acting injectable by GSK ViiV) is priced at $22,000 annually. Such high costs limit access and restrict the global impact of these innovations.
One of the greatest challenges in HIV prevention lies in translating efficacy in results into real-world effectiveness. The timeline from achieving positive efficacy results to regulatory approval and scalable implementation is often prolonged.
Moving an HIV Product to the Real World
Translating positive results into approval and implementation is one of the greatest challenges for medical developments to fight HIV

Years After Efficacy Results
Year Efficacy
Results Obtained
Technology
1
2
3
4
5
6
7
8
9
10
Oral TDF/FTC¹
2010
First regulatory approval
First African regulatory approval
WHO recommendation
Dapivirine
Vaginal Ring
?
2016
First demo project
Technology used at scale
Generic access in LMICs
Injectible
Cabotegravir
?
2020
1 A daily pill consisting of a two-drug combination of tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC)
Chart: Adapted from AVAC by CFR/Allison Krugman

Year Efficacy
Results Obtained
Year of First
Demo Project
Technology
Oral TDF/FTC¹
2010
2016
Dapivirine
Vaginal Ring
2016
2022
Injectible
Cabotegravir
2020
2023
1 A daily pill consisting of a two-drug combination of
tenofovir disoproxil fumarate (TDF) and emtricitabine
(FTC)
Chart: Adapted from AVAC
by CFR/Allison Krugman
The Global Urgency for New HIV Prevention Tools
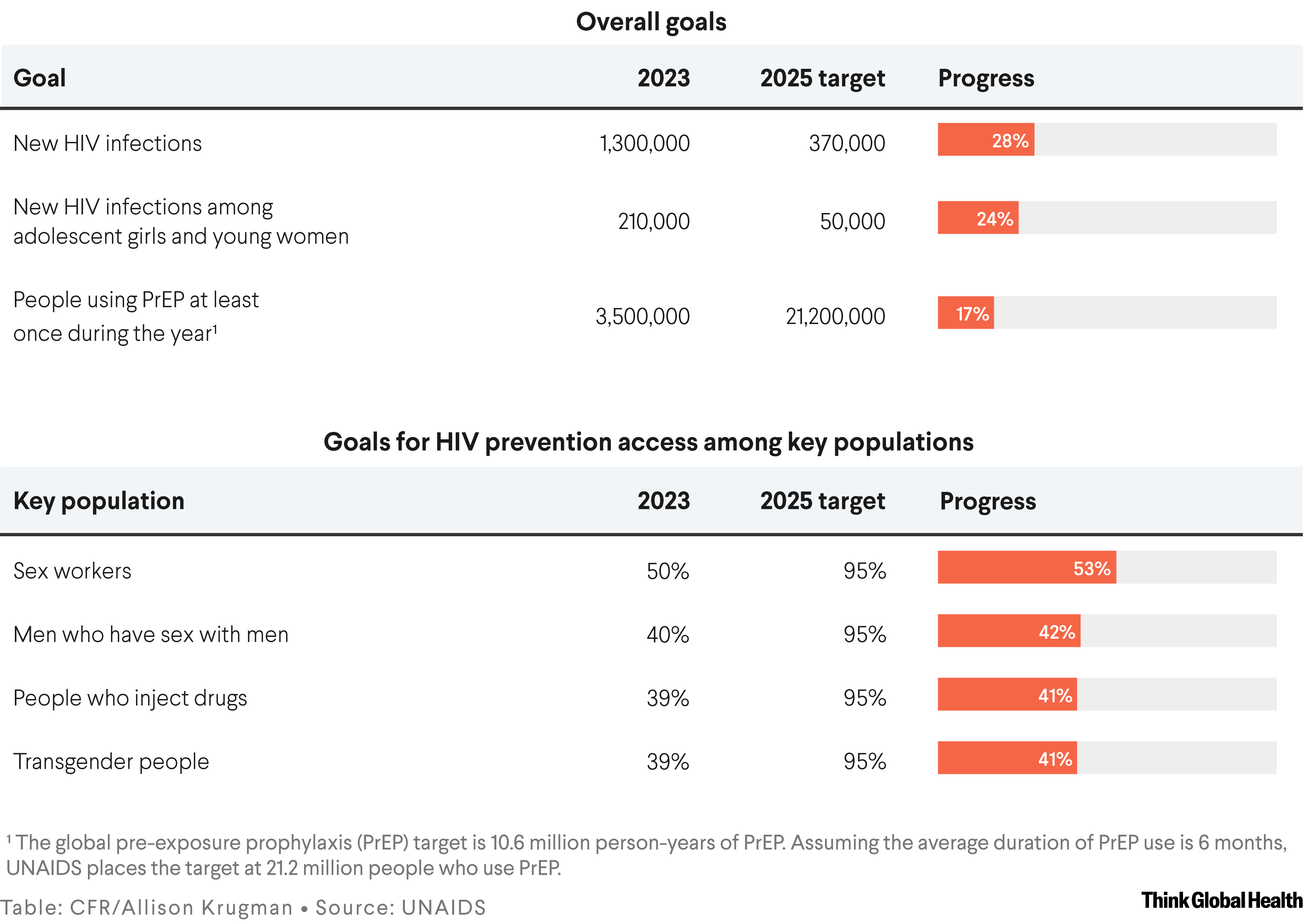
An estimated 1.3 million people contracted HIV in 2023, more than triple the UN Sustainable Development Goals target of fewer than 370,000 new infections by 2025. Despite oral PrEP usage rising from 200,000 in 2017 to 3.5 million in 2023, it remains far below the 10 million user target for 2025. Only 15% of the global need for PrEP is currently met.
The shortfall in PrEP use has critical consequences, particularly for marginalized groups where the disparities are stark and persistent. In sub-Saharan Africa, HIV rates remain high, women and girls accounting for 62% of new infections in 2023. In the United States, 53% of new diagnoses comes from southern states, where only 39% of people eligible for PrEP can access these HIV prevention tools.
Progress Against HIV Is Falling Short
Though more prevention options are available than ever, the world is far from its 2025 targets for HIV elimination
Communities of color, gay and bisexual men, transgender people, and individuals involved in sex work face structural barriers to treatment that include cost, limited health-care access, pervasive stigma, and discrimination. Historical injustices such as the Tuskegee Syphilis Study and the case of Henrietta Lacks have eroded trust in health-care systems among Black communities in the United States in particular, further impeding access.
Balancing Innovation and Access
The case of oral PrEP highlights the dangers of leaving affordability and access unaddressed. Although Truvada and Descovy have been lifesaving for many, high costs and systemic inequities have limited their reach among vulnerable populations. Similar issues afflict cabotegravir, delays in the manufacturing and development of generic versions have hindered its availability, especially in lower-income countries. Even though the World Health Organization recommended cabotegravir for PrEP in 2022, no generic versions will be available until 2027.
The imperative is clear: Combating HIV demands both scientific innovation and strategic economic action. Policymakers, pharmaceutical firms, and global health organizations need to collaborate to dismantle financial and structural barriers. The cost of inaction is immense—not only in human lives but also in long-term economic burdens on health-care systems.
Gilead Sciences has been a trailblazer in HIV research. Although innovation should be rewarded to encourage continued investment, making these breakthroughs accessible to all who need them is a critical challenge. Recent research indicates that lenacapavir could be produced for less than $40 per person annually if multiple generic companies produced it and if the market grew to at least 10 million LEN users. Establishing a fair pricing model would support both innovation and global affordability.
The Shortcomings of Traditional Product Access Models
The complexities of lenacapavir's price structure and persistent global health inequities raise pressing concerns about its accessibility. Traditional reliance on market forces and charitable initiatives has repeatedly fallen short. Market-driven strategies, often guided by profitability, tend to sideline low-income and marginalized communities. Charitable efforts, which often donate product, though commendable, frequently provide only temporary relief without establishing sustainable, long-term solutions.
The complexities of lenacapavir's price structure and persistent global health inequities raise pressing concerns about its accessibility
Tiered pricing, often dubbed Robin Hood Economics, is likely to be applied to lenacapavir. This approach involves pharmaceutical companies adjusting drug prices according to a country's income level. Although intended to improve access in low- or middle-income countries (LMICs) by charging them less and recouping profits from wealthier countries, this approach falls short of ensuring true global equity.
In low-income countries, even reduced prices can be prohibitive due to challenges in separating markets and income inequality, making it more lucrative for manufacturers to target wealthier segments. This is often observed with poor access to oncology drugs in low- and middle-income countries due to the lack of universal health coverage and significant price differences between private and public health-care systems.
These disparities result from inconsistent drug pricing and limited regulatory oversight, making treatments more accessible to wealthier patients but leaving poorer populations struggling to afford essential cancer therapies. In high-income countries, inflated costs strain health-care budgets and benefit pharmaceutical companies more than patients because high prices in wealthier markets often subsidize lower prices elsewhere.
Leveraging Voluntary Licensing, Volume Guarantees, and Public-Private Partnerships
On October 2, 2024, Gilead announced its commitment to issuing voluntary licenses to generic manufacturers, a crucial step to ensuring broad access. This involves granting nonexclusive licenses to multiple generic producers before regulatory submissions, which could reduce the time to market for generic products. The price tag is still unknown, but the cost analyses suggest that with generic competition, lenacapavir's price could drop below $100 per person annually, potentially plummeting to $41 for enough to treat 10 million people for 1 year. Also, some high-incidence countries hosted PURPOSE 2 trials of lenacapavir are excluded from current licensing geographies.
This brings the point of granting provisions focused on public health, ensuring access based on need rather than geography or income. Additionally, generics may take a few years to come to market, partially given the need for bioequivalence studies.
Collaboration with entities such as the Medicines Patent Pool, which has successfully facilitated licensing for other critical medications, could allow more transparency regarding the process of licensing to generic manufacturers. However, effective voluntary licensing demands careful partner selection, stringent regulatory oversight, and robust legal frameworks to ensure both quality and accessibility.
Beyond pricing and licensing, innovative financing mechanisms such as volume guarantees and public-private partnerships offer pathways to enhance lenacapavir's accessibility. Volume guarantees provide a promising alternative or complement to tiered pricing; by ensuring a minimum purchase quantity, manufacturers can lower prices through economies of scale. For example, during the COVID-19 pandemic, a collaboration between the nonprofit MedAccess, the Clinton Health Access Initiative, and the biotech company Wondfo resulted in a $1 HIV self-test for LMICs using a volume guarantee.
Public-private partnerships can reduce costs by focusing on product registration, local production, and integration into national policies. A notable example is the collaboration between the Children's Investment Fund Foundation and the Global Fund, which recently committed up to $2 million to purchase 150,000 dapivirine vaginal rings, a long-acting HIV PrEP option for women. However, this initiative does not directly reduce the price of the rings; instead, it aims to enhance access and create a more sustainable market for these vital prevention tools.
By bridging the gap between discovery and delivery, partners—including governments, pharmaceutical companies, global health organizations, and communities—can transform obstacles into opportunities, turning the tide of the epidemic. The potential for progress is immense but requires a collective commitment to making equitable access a reality for all.













