Since the first COVID-19 vaccines became available, U.S. policymakers have tried to ensure those at highest risk of death were vaccinated first, prioritizing groups such as older adults and those with multiple pre-existing conditions. But the racial and ethnic minority groups at highest risk of mortality were absent from CDC guidelines, and only a few states placed in these groups at the front of the vaccination line. Subsequent rates of vaccination have been starkly inequitable across racial and ethnic lines, and the spread of new variants across the United States could deepen these disparities. As states open vaccination to all adults, they must take steps to ensure that all racial and ethnic communities have the information and access necessary to protect themselves from COVID-19.
Compared to the national average, racial and ethnic minority groups have experienced five times the incidence of COVID-19 deaths
Compared to the national average, racial and ethnic minority groups (including Hispanic or Latino, non-Hispanic American Indian or Alaska Native, non-Hispanic Black, and non-Hispanic Native Hawaiian or Other Pacific Islander individuals) have experienced five times the incidence of COVID-19 deaths, elevated across nearly all age strata and with the greatest disparities among non-Hispanic American Indian and Alaska Native individuals. If every American shared the mortality rate of non-Hispanic American Indian or Alaska Native individuals of the same age, instead of 561,000 COVID deaths, we would have seen 1.29 million deaths nationally by April 13. Age is the most prominent risk-factor for severe COVID-19 symptoms, but risk in some racial and ethnic minority communities is so high that individuals in those groups are facing comparable odds to non-Hispanic white individuals 10 to 15 years older. For example, Hispanic or Latino people under 35 have a risk of mortality similar to non-Hispanic white people who are 35 to 44 years old.
In the early phases of their vaccination distribution program, many states, including Massachusetts, New Hampshire, and California, prioritized counties that were disproportionately affected by the pandemic, or allocated additional vaccines to vulnerable and disadvantaged communities. But only a few states, such as Montana and Utah, prioritized American Indians and people of color. By not prioritizing racial and ethnic minority communities for vaccination, most states missed an opportunity to focus on the racial and ethnic groups that were at highest risk.
U.S. COVID-19 Mortality Rates by Race and Ethnicity
Reducing these inequities in COVID-19 outcomes will require us to address deep-seated impacts of systemic racism, but much can be done immediately to alleviate some of the disparities. Broadly, we need to rethink the concept of vaccine "access." Expanding eligibility for vaccination is only the first step in ensuring access; public health entities must also ensure everyone has the necessary information to judge vaccines' safety and acceptability. Several polls and surveys show that a substantial share of the population remains hesitant to be vaccinated, and this hesitancy is more pronounced among communities of color. Common concerns include worries about serious long-term side effects; a desire to learn more about vaccine safety and efficacy; and lack of trust in the medical and government institutions responsible for vaccine development, approval, and administration.
COVID-19 Deaths per 100,000 by Age Cohort
COVID-19 deaths are compared between non-Hispanic white people and Hispanic or Latino people
These concerns are not unfounded: mistrust in the U.S. health system reflects decades of medical mistreatment that continues today, as seen in the case of Dr. Susan Moore, a clinician in Indiana who died from COVID-19 after reporting racist treatment by health-care workers. To ensure that hesitant individuals are able to make informed decisions about COVID-19 vaccination, all racial and ethnic communities deserve access to scientifically accurate, culturally appropriate, and linguistically accessible information regarding the community- and individual-level risks and benefits of vaccination. Critically, this information must come from sources trusted by the particular community in question.
Even individuals who say they want to be vaccinated immediately face additional structural barriers. Although the vaccine itself is free, transportation and missed work hours—either missed when attending a clinic or when staying home as a result of vaccine side effects—present additional financial barriers. Additionally, polls indicate that Hispanic or Latino respondents and non-Hispanic Black respondents are more likely than non-Hispanic white respondents to express concern about finding transportation to a vaccination site or missing work because of vaccination. Facilitating transportation to vaccine sites and keeping clinics open nights and weekends could help alleviate this financial burden. And although the vaccine is available to people regardless of immigration status, undocumented individuals may be reluctant to seek government-sponsored vaccination for fear of legal repercussions. To support vaccination access in these communities, officials should work with people trusted by the community they are serving.
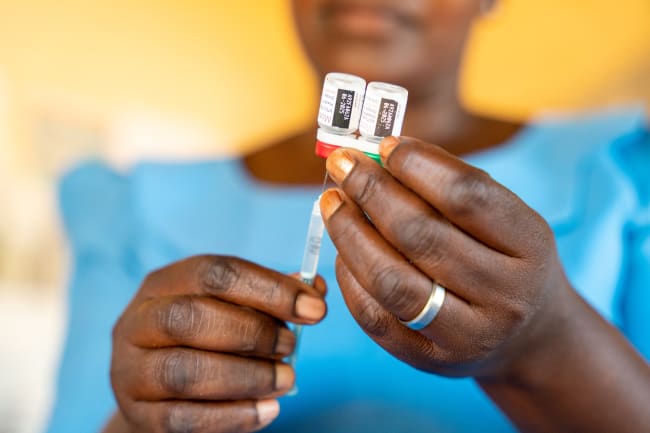
All racial and ethnic communities deserve access to scientifically accurate, culturally appropriate and linguistically accessible information
As new viral variants spread, it is critical to get as many individuals vaccinated as rapidly as possible. Targeting vaccine distribution efforts to groups that are at highest risk of severe outcomes is just one step in reducing COVID-19-related inequities. If and when booster vaccines become available to protect people against variants, all locations should follow the example of the few states that prioritized vaccines for the racial and ethnic groups with higher risks of death.
Vaccines are an invaluable tool for protecting individuals and communities, particularly those who lack access to quality health care. There is an immediate need to develop and deploy targeted efforts to bring vaccines and accurate, context-appropriate information about their safety to those who need them most.

EDITOR'S NOTE: The authors are employed by the University of Washington's Institute for Health Metrics and Evaluation (IHME), which produced the COVID-19 forecasts described in this article. IHME collaborates with the Council on Foreign Relations on Think Global Health. All statements and views expressed in this article are solely those of the individual authors and are not necessarily shared by their institution.