As SARS-CoV-2, the virus that causes COVID-19, continues to spread, the ongoing pandemic continues to place a heavy burden on health workers, health systems, and the global economy. The capacity of health systems—how many providers, facilities, beds, equipment, and supplies are needed to treat routine and critically ill patients—have been scaled up.
Surgical and anesthesia professionals and systems have seen 400 to 500 percent increases in critical-care demand
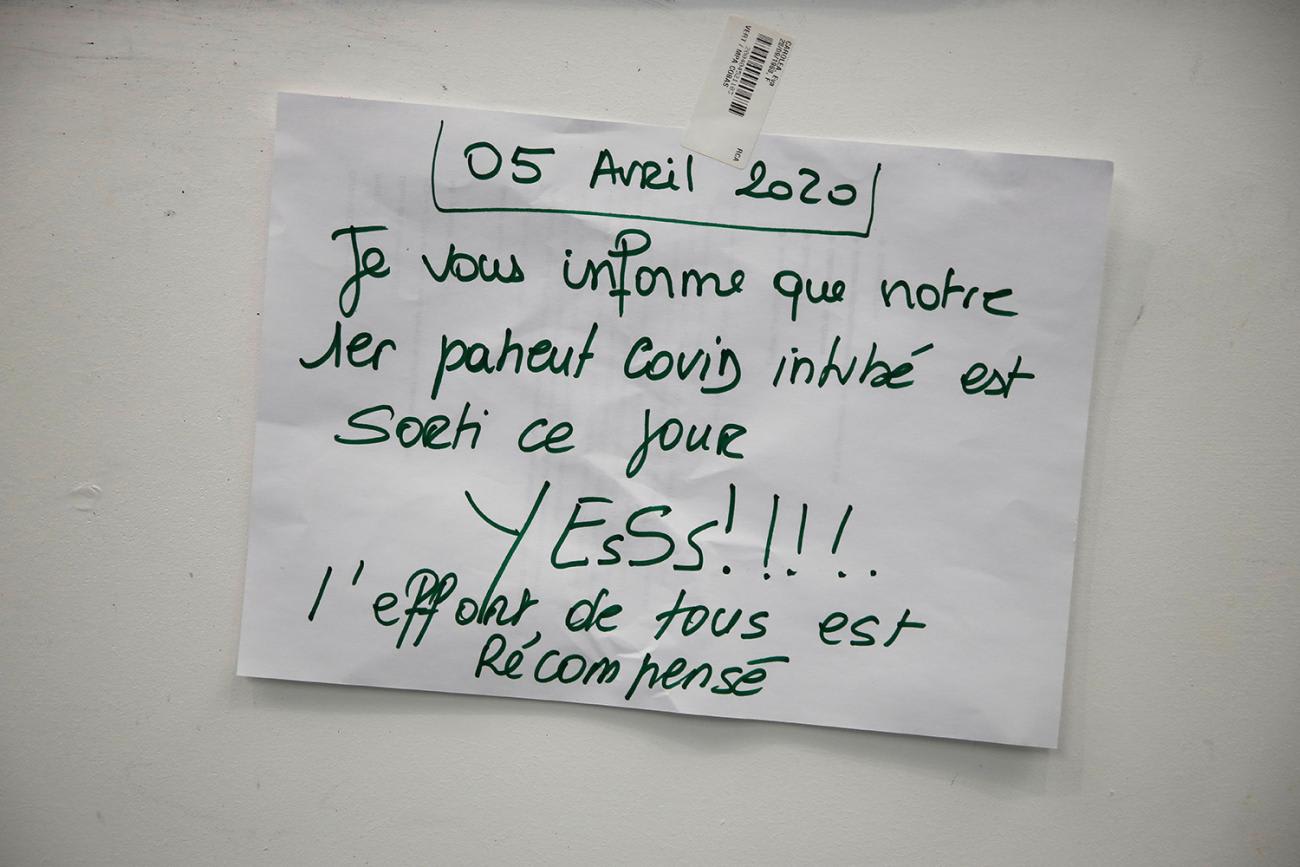
Countries have had to respond quickly in the last nine months to make access to critical care, including surgery and anesthesia, a priority during the COVID-19 pandemic. Responding to the need for urgent care in countries around the world with limited resources and capacities, hospital administrators and providers in those countries acted swiftly, even converting operating rooms and post-operative care units into bed wards for moderately and severely ill people with COVID-19. Surgical and anesthesia professionals and systems, both essential to the pandemic response, have seen 400 to 500 percent increases in demand for critical-care services.

This critical-care scale-up in response to the pandemic provides an important opportunity to think about long-term global needs for universal access to surgery and anesthesia, to consider how we can meet those needs, to bring new investments in order to do so, and to improve health system resilience worldwide.
Why Surgery and Anesthesia Are Essential for Treating COVID-19
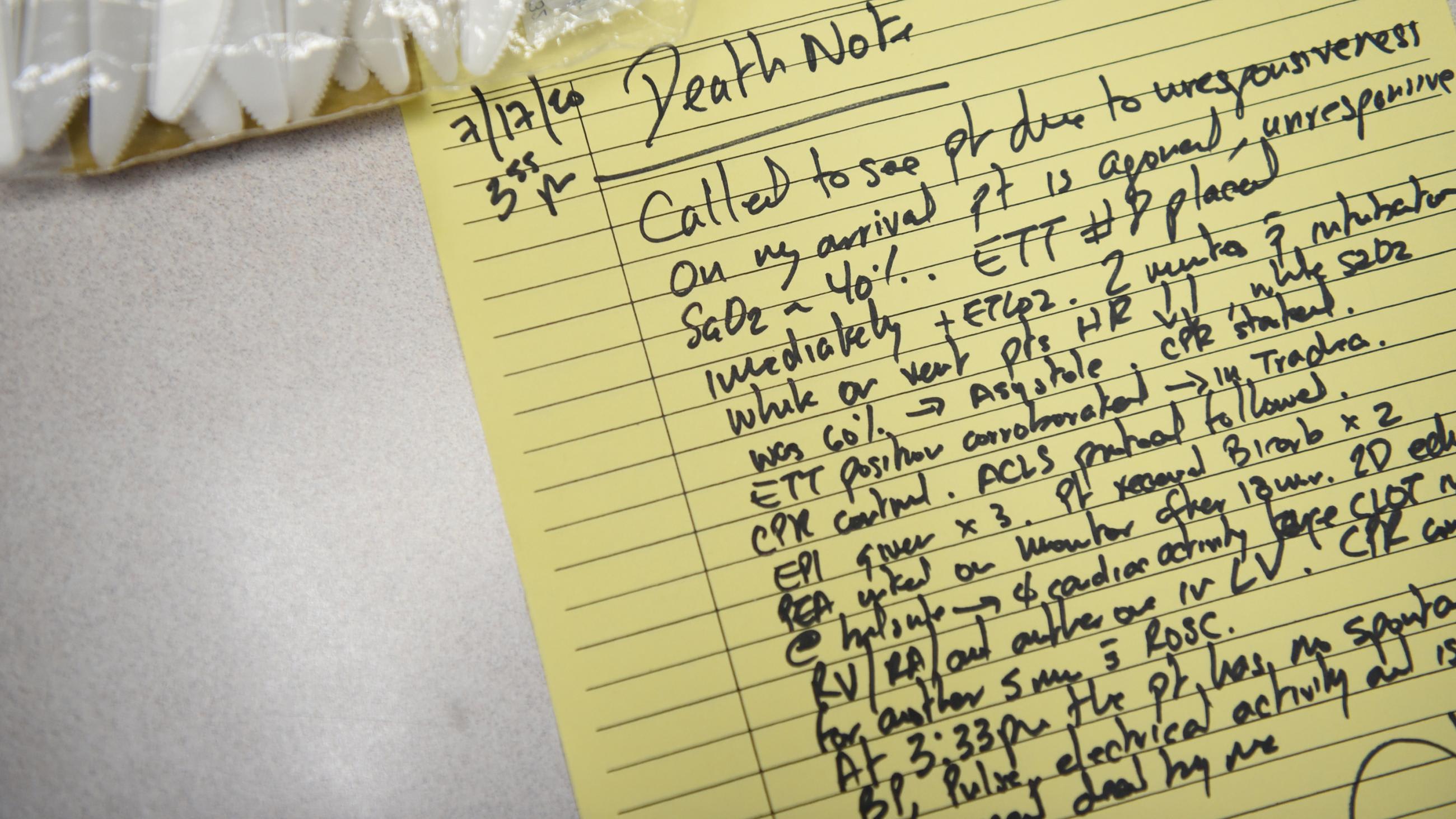
Because the coronavirus can trigger an upper or lower respiratory tract infection, affecting the nose, throat, sinuses, trachea (windpipe), and lungs, anesthesiologists are often called on to treat people with COVID-19.

When the virus settles in the lower airways, inflammation of the lungs can lead to pneumonia and acute respiratory distress syndrome, a severe and deadly form of lung failure. Managing critical COVID-19 cases often requires giving people support for their breathing and increasing their oxygen levels. This often requires the intubation of patients who can no longer breathe on their own and need to be aided by a mechanical ventilator—a procedure that has become familiar to even the non-clinical public during the pandemic. Intubation carries a high risk of infection because it involves inserting a tube, called an endotracheal tube, through the mouth into the airway, often causing the patient to cough out virus-laden, aerosolized particles in the process.
Often causing the patient to cough out virus-laden, aerosolized particles
Intubation—and much of the work of managing the treatment for COVID-19—relies on the skills of experienced anesthesia providers to care for critically ill patients and monitor their mechanically-assisted breathing. Around the world, these providers have developed innovative solutions for airway management to prevent infection and conserve scarce resources, like using a single ventilator for multiple patients or retrofitting alternative equipment. Anesthesia providers have also been responsible for training non-anesthesia specialists in the care of these sickest of patients when hospitals experienced staff shortages, and international organizations like the World Federation of Societies of Anesthesiologists (WFSA) developed specific new guidelines for anesthetic and critical-care management in COVID-19 patients.

Building Critical-Care Capacity In Poorer Countries
Globally, an estimated 5 billion people (including 1.7 billion children) have no access to safe, timely, affordable, and often medically necessary surgical and anesthetic care. In countries with limited surgical capacity, anesthesia care is also severely limited, with many countries having less than one physician anesthesia provider per 100,000 people. Compare this with a minimum acceptable number of five providers per 100,000 people, recommended by the World Federation of Societies of Anesthesiologists
Globally, an estimated 5 billion people (including 1.7 billion children) lack access to surgical and anesthetic care
Because of gaps in surgical and anesthesia care, governments in many low- and middle-income countries preparing for their COVID-19 responses have experienced insufficient, and sometimes nonexistent, access to crucial oxygen, ventilators, personal protective equipment (PPE), critical-care beds, and providers with the experience to handle an influx of patients with severe disease. Further complicating the pandemic response, the number of surgeries in low- and middle-income countries represents a small proportion of the global surgical volume. The vast majority of surgical need in these countries goes unaddressed due to limited resources and, as a result, most of the surgeries performed in these countries are emergency procedures. The consequences of canceling or postponing these cases to make room for critical-care patients, as was widely done with elective procedures in high-income countries, would be devastating.

Challenges in surgery, anesthesia, and critical-care capacity in low- and middle-income countries during the COVID-19 pandemic were addressed in a recent webinar during the United Nations General Assembly, hosted by the Global Alliance for Surgical, Obstetric, Trauma and Anesthesia Care (G4 Alliance), the Harvard Medical School Program in Global Surgery and Social Change, and the Global Initiative for Children's Surgery.
The vast majority of surgical need in these countries goes unaddressed
Experts from around the world—Canada, Honduras, Indonesia, Kenya, Nigeria, the Philippines, the United States, and other countries—described how their governments and health systems embarked on a rapid scale-up of critical-care capacity, where it was possible. This has included local production of PPE when supply chains became stressed due to heightened demand in Europe and North America, extensive health worker training and redeployment, better health team integration, implementation of virtual learning and telemedicine, and real-time epidemiological studies of the impacts of COVID-19 on surgery.

Additionally, adaptations were made to basic anesthetic approaches. Regional anesthesia involves the delivery of targeted local anesthetics at specific nerves and nerve groups. This is in contrast to what is often referred to as local anesthesia, meaning simple infiltration of a smaller area with local anesthetic (e.g. removal of a mole). Thus, regional anesthesia has the ability to target nerves that will render larger areas of the body, such as an entire limb, adequately anesthetized (i.e. numb) for surgical procedures (e.g. treatment of an open leg fracture).
A potentially cost-effective pathway for expanding anesthesia services in less-resourced healthcare settings
Regional anesthesia is a technique that is sometimes an alternative to general anesthesia, as a regional technique often does not require invasive airway management (e.g. intubation) to aid breathing. Regional anesthetics, as opposed to general anesthesia, can reduce risk from aerosolized particles, reduce the use of scarce medications needed for intensive care, and reduce the use of PPE needed in caring for people with COVID-19. Even before the pandemic, many providers in low- and middle-income countries were trained to perform regional anesthesia, according to Celeste Quan of the Chris Hani Baragwanath Academic Hospital in South Africa. Quan also noted that, because regional anesthesia requires fewer materials and drugs, this approach presents a potentially cost-effective pathway for expanding anesthesia services in less-resourced healthcare settings. However, there is still a significant service gap in many facilities.
Lessons learned during this pandemic—such as the value of regional anesthesia and ability of anesthesia providers to adapt to care for critically ill patients in a variety of settings—must be carried forward. The current pandemic demonstrates unequivocally that investments in surgical and anesthesia systems today mean that health systems can shift to crisis management in the future without sacrificing essential surgical care.
Critical-Care, Surgery and Anesthesia
Dramatic expansion of surgical and anesthesia capacity in low- and middle-income countries is achievable, and doing so would save many lives. Important foundational elements are being developed now—even in the midst of a pandemic—as part of critical-care systems.
Yet without additional support, we risk continued, difficult tradeoffs between crisis response and emergency and essential surgical and anesthesia care.
Now is the time to realize two goals: global health security and universal access
It would be a sadly missed opportunity for proponents of health systems strengthening and supporters of the United Nations' Sustainable Development Goals not to expand upon these existing investments of valuable health-care resources. These resources and commitments can be leveraged to scale surgical and anesthesia care through integrated national health planning and funding, while also preparing for the next pandemic or crisis. Governments have demonstrated that they can quickly and efficiently implement this scale-up through newly-formed channels for funding, critical-care management, and adaptive learning. Now is the time to realize two goals at once: global health security through responsive health systems and universal access to essential surgical and anesthesia care.












