This month, world leaders will gather at the UN General Assembly to address the looming threat of antimicrobial resistance (AMR). They will discuss antimicrobial access, governance, coordination, and many other critical aspects of the fight against AMR.
Yet there's one critical component to any successful outcome that is overlooked and underfunded: the dwindling antimicrobial research and development field.
Antimicrobial researchers are the backbone of the antibiotic innovation needed to keep everyone safe from increasing antimicrobial resistance. They pioneer new treatments on a perpetual basis, overcome the challenges associated with resistance, and ultimately drive public health. Without a healthy market for antibiotics, their career paths and longevity in the field are under threat. Many are moving into other areas of research.
AMR ranks as a top 10 global health threat and was responsible for 1.27 million deaths worldwide in 2019. Unless action is taken to bend the curve, it is on track to cause as many as 10 million deaths every year by 2050 at a cumulative cost of $100 trillion of global GDP. Although stewardship efforts and public health initiatives help counter AMR, the urgency, coordination, and investment needed to deliver new antimicrobial treatments—the strongest antidotes to resistant bacteria—are still missing.
As a result, the AMR field has been steadily losing vital scientific and research talent for more than two decades. The research and development (R&D) pipeline is thin and no treatments are in development for more than half of the most concerning bacteria classed as innovative. This raises a question. Even if world leaders find the will to spur antibiotic innovation at the UN's high-level meeting, who will deliver the necessary drugs?
A Broken Marketplace
The market for new antimicrobials doesn't attract investment. Unlike other drugs, antimicrobials face a unique dilemma: Because using them improperly opens the path to resistance, new antimicrobials should be used only when needed, which limits sales volumes. When revenue is tied directly to sales, the economic logic of further investment is upended.
On top of that, standard approaches to valuing antimicrobials do not work because they miss the population protection benefits of being ahead of emerging resistance. The United Kingdom's National Institute for Health and Care Excellence (NICE) recently rolled out an innovative valuation model that captures the deficit, but other countries have not yet adopted similar approaches. This further disincentivizes companies from investing in the long-term, risky R&D needed to produce new drugs.
Even if world leaders find the will to spur antibiotic innovation at the UN's high-level meeting, who will deliver the necessary drugs?
The AMR Industry Alliance's research found that multiple new antibiotics were introduced each year in the 1980s and early 1990s. Since then, new drug releases have declined sharply. Roughly one new antibiotic has been introduced each year since the early 1990s.
Moreover, the companies that have successfully launched 7 out of the last 10 antibiotics no longer exist, having gone bankrupt or been purchased at knockdown prices. Consider the case of Achaogen. It secured approval for plazomicin, an antibiotic used to treat complicated urinary tract infections but was still forced to declare bankruptcy after investing a billion dollars and 15 years developing the antibiotic.
This cycle not only hurts the smaller biotech companies, but also affects the major pharmaceutical companies as well. Several larger companies have cut back on AMR research and funding despite the increasing burden of AMR in low-, middle-, and high-income countries.
Much of the remaining antibiotic R&D is done by small- and medium-sized enterprises, which face severe challenges raising the necessary investment. According to a report from the BEAM Alliance, 54% of these businesses don't have enough funds to cover a year's worth of operations—some 33% reporting less than 200,000 euros ($222,000) cash.
Circling the Brain Drain
In addition to heavy investment, it takes time, experience, skill, and talent to build a high-quality team of researchers. But it is becoming increasingly difficult to build one. Many experts with essential knowledge have already left the field in response to cost pressures, limited incentives, and a lack of compelling opportunities—not to mention fear of their employer's going bankrupt or shuttering the operation.
Simply put, the AMR brain drain threatens every part of the drug development process, from basic discovery research through clinical testing all the way to regulatory approval and life-cycle management.
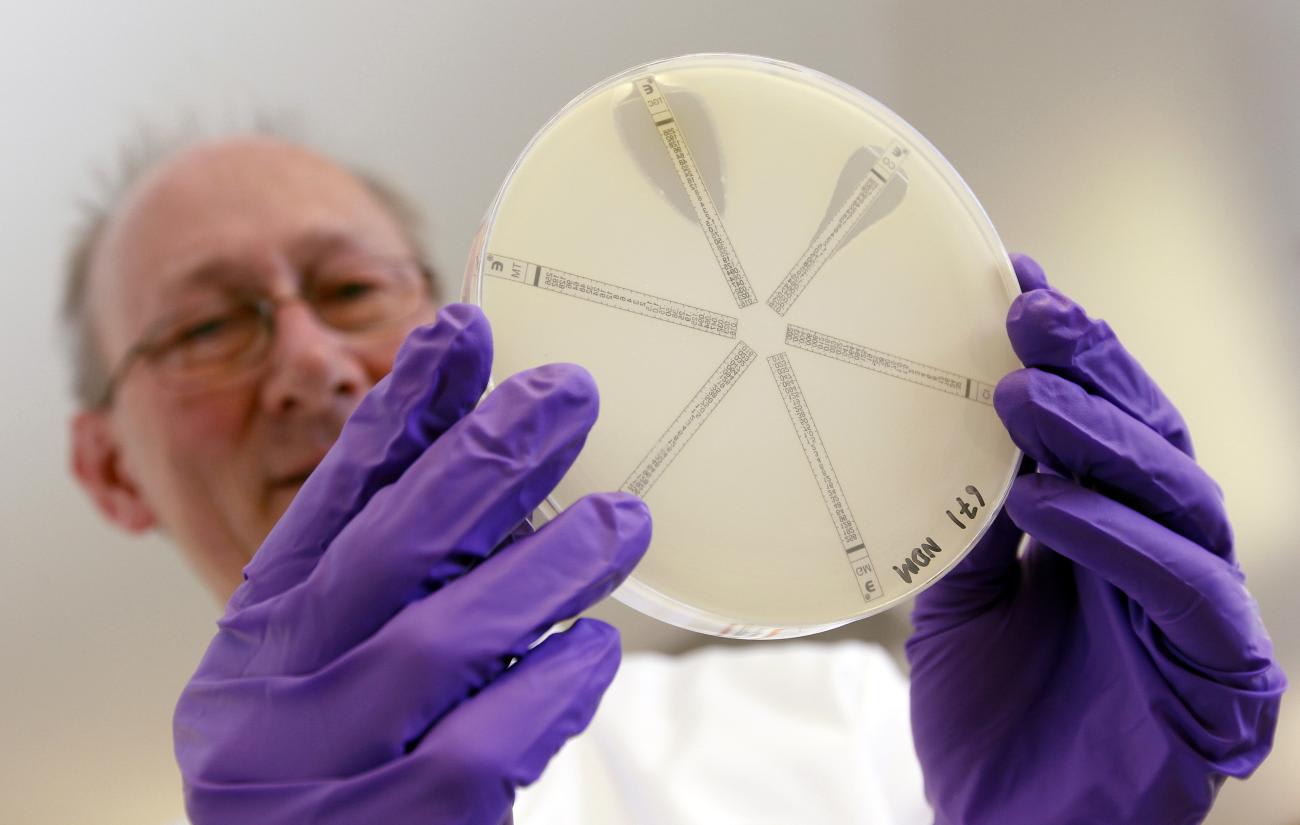
The AMR Industry Alliance research identifies approximately 3,000 AMR researchers relative to 46,000 for cancer and 5,000 for HIV/AIDS. Authors of AMR publications—a good proxy for experts in the lab—halved from 1995 to 2020, and researchers with three or more publications fell by roughly the same amount. That exodus appears to be unique to antimicrobials. In 2022, academic journals published approximately 5.5 times more on HIV/AIDS than priority bacteria, even though AMR is estimated to contribute to more deaths every year than AIDS.
Unfortunately, this problem is not confined to researchers. Clinicians are a crucial part of the antimicrobial and antifungal R&D teams. Yet in the countries where AMR-related R&D takes place, infectious disease specialist numbers are low, and few new specialists are entering the field.
In 2022, 44% of the infectious disease (ID) fellowships in the United States went unfilled—more than double the proportion of unfilled fellowships across all specialties. Nearly 80% of U.S. counties either do not have ID physicians at all or have below average ID physician density.
A Path Forward
Fortunately, many of the researchers and experts left in the AMR field remain interested, engaged, and passionate about their research. They are the field's greatest strength and a critical resource for the future. Policymakers, pharmaceutical companies, biotechs, government procurers, and all AMR-focused stakeholders alike need to fix the broken market to ensure AMR researchers can continue their vital work and train our next generation.
Fortunately, many of the researchers and experts left in the AMR field remain interested, engaged, and passionate about their research
The main solutions are economic. I'm proud that within the AMR Industry Alliance, which I chair, 34 members have invested $2 billion on average annually in AMR-relevant research and development. The private sector, though, can take us only so far. Governments and other stakeholders need to create a more sustainable market for antimicrobial products. If no action is taken, the pipeline will continue to decline and researchers will continue to depart for other work.
One way to do that is by changing the economic logic of the market. The United Kingdom has forged an innovative model among Group of Seven (G7) countries in fighting AMR. Its National Health Service recently introduced a subscription-based model that separates revenue from sales volume. A subscription model provides the government with the antibiotics it needs when it needs them; meanwhile, companies receive the revenue and predictability they need to recoup their investment and continue research, regardless of how many pills are sold each year. If similar models are adopted across the G7, industry modeling suggests that the research pipeline will increase significantly over the next decade.
Public funding for research and derisking private-sector investment can also help. Organizations such as CARB-X are stepping up to support several dozen small companies, giving them and their researchers a critical lifeline to continue their important work. The $1 billion AMR Action Fund was launched in 2021 to offer a short-term funding bridge for innovative antibiotic companies and has invested in seven so far. Efforts like those should be encouraged by governments and other funders.
Ultimately, to meet the need for new antimicrobials that can stay ahead of the resistant bacteria, both the public and private sectors should invest in the people who are responsible for the discovery of antimicrobials to attract and retain the best scientists into the future.













