Editor's Note: This article is adapted from a blog post at Resolve to Save Lives that summarizes a series of tweets sent by the author at the end of last week—a regular weekly round-up on the COVID-19 pandemic, with a focus on the latest epidemiological data in the United States. Last week's tweets focused on the turning tide, which is still too high to warrant any sighs of relief. The author calls for a continuously improving response. "The better we understand the virus, our risk, and our response with real-time, strategic intelligence, the better we can fight it," he said.
COVID-19 positivity continues to be high among 5-17 year-olds—higher than 10 percent among those tested in the age group
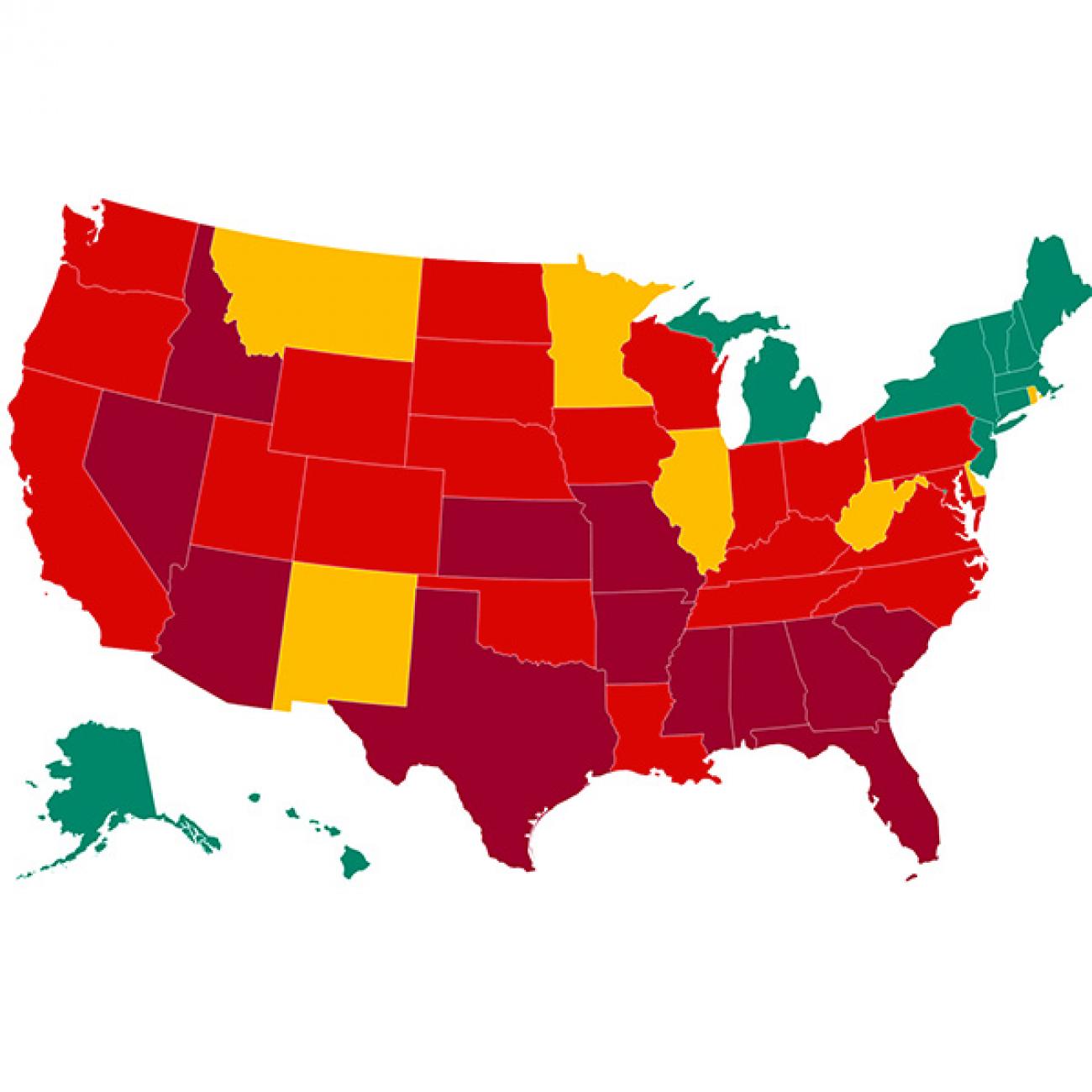
Decreasing test positivity rates and cases in many areas indicate that the tide is beginning to turn in the United States. Positive tests were down nationally last week, from 8.7 percent to 7.8 percent, including decreases across all lab types in nine of ten regions. But it’s still very high—too high in many places. Will we relax control measures too soon—again—before we have the virus on the run and we’re able to corner it? Surprisingly, positivity continues to be high in 5-17 year-olds. It’s greater than 10 percent among people tested in this age group, which is the highest of any age group. Some locations also have persistently high positivity rates. Any place that has a positivity rate above 5 percent has lots of COVID-19, probably too much to be able to open schools and keep them open safely.

It's not just about having enough tests, it's about having fewer cases. Unless we decrease spread, we'll never have enough tests. And when we decrease spread, we need to use tests to quickly isolate infectious people and warn their contacts before they infect others.
We shouldn’t pay for tests if they take more than seventy-two hours to come back
Remember: a test alone does nothing to control COVID-19. It’s only useful if it results in rapid isolation of infectious people and rapid warning and quarantine of contacts. We shouldn’t pay for tests if they take more than seventy-two hours to come back. Tying payments to test turnaround time is a healthy incentive for companies to get test results back faster. For example—and Bill Gates also suggested this—if a test comes back after forty-eight or seventy-two hours, pay nothing. Maybe pay more if it comes back within twenty-four hours. And every state should report on how long it takes for test results to be returned.

One potential approach to controlling COVID-19 re-calibrates the number of tests needed to keep positivity below 3 percent. This is what the folks at www.covidexitstrategy do on their home page. By that measure, the United States, which last week averaged 740,000 tests with 7.4 percent positivity, would need more than twice as many to be doing anywhere near enough.
If everyone sticks to public health recommendations and mandates, we can drive cases down by 80 percent
If everyone sticks to the three W’s and public officials mandate closure of indoor places where COVID-19 spreads (such as bars), we can drive cases down by 80 percent, meaning many fewer tests would be needed. Wear a mask (more data is coming out that surgical masks are much more effective than cloth face coverings—and there is no reason we can’t make plenty of surgical masks in this country). Wash your hands (debates about contaminated surface versus aerosol spread continue and are very difficult to resolve with science, but both are risks, all three W’s are important). And watch your distance (even with masks on, avoid crowded indoor places—especially those with poor ventilation).

We’re seeing big decreases in the number of tests reported from Texas, Florida, Washington State, Minnesota, and Puerto Rico. What’s happening? The average daily tests nationally decreased by more than 40,000 last week, driven by a decrease of nearly 60,000 in the above five places, despite increases elsewhere in the United States.
Test positivity tracks disease rates reasonably well not only in the United States, but also globally. We’re a long way from where we need to be here and in many parts of the world. Latin America continues to get hit hard, as do parts of Africa and Asia and the Middle East.

Another important indicator is flu- and COVID-19-like illness visits to emergency departments, which continue at low and stable levels in all regions of the United States. In most years, flu doesn’t begin to hit hard until January. With less global travel and more physical distancing, flu season could be milder this year. That’s what South Africa is seeing so far, and this is usually their flu season. But by all means, get a flu shot this fall. We don’t know what flu season will be like this year, but every season is now COVID-19 season.
We are nowhere near herd immunity, and getting there would mean at least a million people dead in this country alone
Deaths remain high and increased to approximately one death per minute in the United States last week. We are nowhere near herd immunity, and getting there would mean at least a million people dead in this country alone. The unique U.S. failure to control COVID-19 isn’t just that the United States has more deaths than any other country—or among the highest death rates in the world. It’s that countries in Europe and elsewhere have a handle on their epidemic and a tiny fraction of the deaths per day we are having now. People living in Europe had about one eighth the chance of being killed by COVID-19 last week compared with people in the United States. Virtually every model and projection suggests that the United States will have more than 650 deaths per day through the end of August. We must not lose sight of the horror of these numbers. These deaths are unacceptable, preventable tragedies. Will COVID-19 be a new, tragic example of American exceptionalism, or will we join together, physically distanced, to stop the virus?

In Africa and elsewhere, interrupted vaccinations and forced delays or interruptions in treatment of HIV/AIDS, tuberculosis, and malaria could mean more deaths from COVID-19 disruption than from COVID-19 infection itself. This possibility—of literally millions of deaths because of the disruption of COVID-19—scares me more than anything else about the pandemic. We must protect health workers and health care.
There is an encouraging start by the U.S. Centers for Disease Control and Prevention (CDC), an agency I formerly led, on a science-based approach to vaccination, respecting communities. A vaccine is the most important future tool to fight COVID-19, but it’s not going to end the spread of COVID-19 any time soon. The virus is here to stay, and our response must improve continuously.

It's not that complicated.
- Close places where COVID-19 spreads. Bars, indoor dining, choirs, etc.
- Test-isolate-trace-quarantine. Repeat until you’re finding and stopping most transmission.
- Wear a mask, wash your hands, watch your distance.
- Learn more about the virus and how to stop it.
The virus will exploit every weakness it can find that divides us
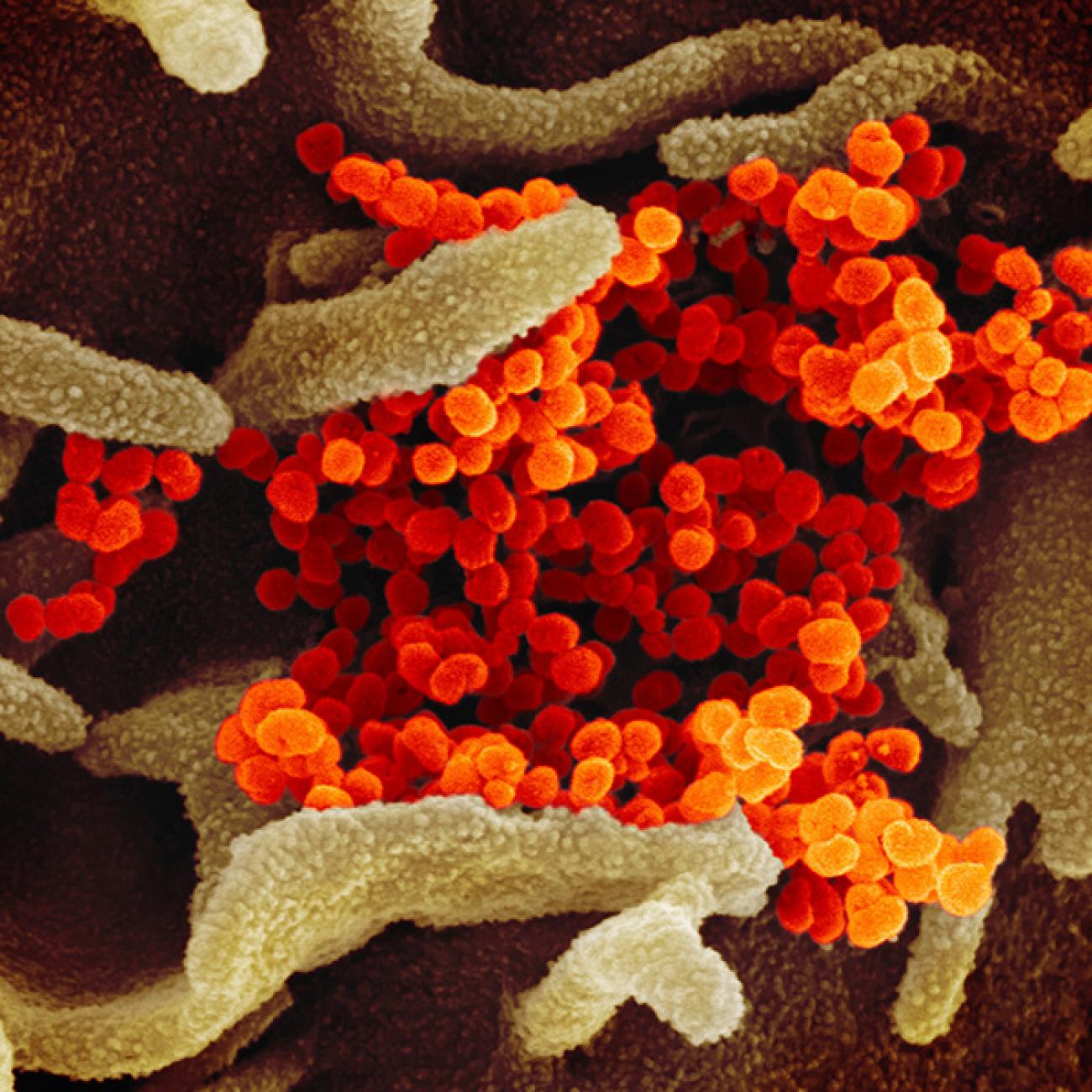
There’s only one enemy here, and that’s the virus that causes COVID-19. The virus will exploit every weakness it can find that divides us. The coronavirus thrives in societal fault-lines of partisanship, systemic racism, inadequate care of the elderly, weak infection prevention and control in health-care facilities, unhealthy conditions in correctional facilities, homeless shelters, factories, lack of support for primary care, and more. The better we understand the virus, our risk, and our response with real-time, strategic intelligence, the better we can fight it.