In the nearly four years since Chikwe Ihekweazu became Director-General of the Nigeria Centre for Disease Control, his agency has had to deal with numerous infectious disease outbreaks. His team responded to thousands of cases of Yellow Fever; a severe outbreak of meningitis that affected more than 14,000 people; several cases of polio; a massive surge of Cholera that struck 43,000 people in 2018; the first cases of monkeypox in decades; and the largest outbreak of Lassa fever in history. Now novel coronavirus threatens Africa as well as the rest of the world. Last week, just before the first case of COVID-19 was detected in the country, Think Global Health sat down for a phone interview with Ihekweazu, to talk about where things were going with COVID-19 and other infectious diseases in Nigeria and the rest of the continent.
□ □ □ □ □
THINK GLOBAL HEALTH: How prepared is Nigeria and West Africa in general for COVID-19, and what should people outside the region know about your preparedness?
IHEKWEAZU: I think our biggest area of vulnerability—and it's an area that no one really quite knows how it will pan out—is if we do have established circulation, transmission in Nigeria, what level of clinical care do we need to provide for patients?
If you do have widespread transmission in Nigeria, the biggest risk will be our ability to provide clinical care… that's what I worry about the most
If you think about the numbers of people infected and the proportion of those who end up being severe—even though the proportion is fairly small, based on data out of China—the absolute numbers will be fairly significant if transmission really gets a foothold in a context like Nigeria. So our best bet is to really focus as hard as we can on early detection, and to ensure that we have the capabilities to maintain and contain the size of transmission to a limited number of cases. Because if you do have widespread, established transmission in Nigeria, the biggest risk will be in our ability to provide clinical care. That includes ventilators and oxygen therapy to a large number of patients, and that's what I worry about the most. So we really have to focus on the hardcore public health and prevention [approaches] of early detection and early response in order to limit transmission in a context like ours.

I think people should respect the progress that has been made on this continent and the hard work that has gone into making that progress. We do need help and support. But at the same time, we have focused, especially since the Ebola outbreak of '14-'15, on building national public health institutes, building laboratory capacity, developing leaders across our sector, and coordinating among ourselves a lot better than has ever been the case.
There are specific bottlenecks that we need to work together as a global community to improve—the one obvious one is access to diagnostics. A lot of the diagnostics that we need are simply not easily accessible, and there's no commercial interest in developing them. The whole manufacturing process have been defined for a certain market in the world where a lot of these diseases no longer happen.
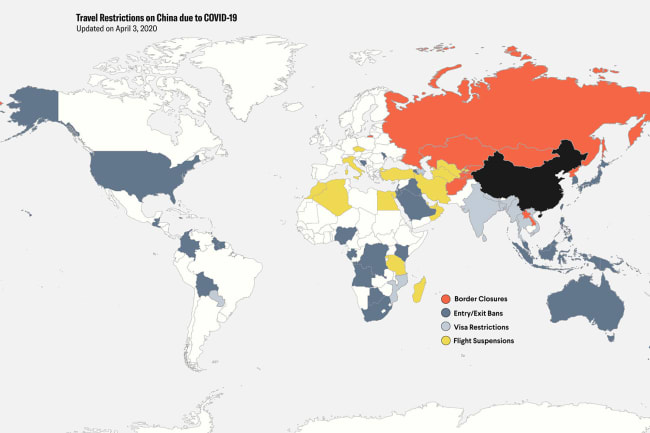
The concept of every country trying to look only within its own borders is completely, mindbogglingly, a waste of everybody's time
If we all say that we live in a global village, and health security is everybody's problem, then why are we not developing our response with that notion in place? You can't say that global health security is everybody's problem, yet within the global system access to diagnostics, access to therapeutics, access to vaccines is managed through a pathway that limits the access to parts of the world, because inevitably we put ourselves collectively at risk. I think that our whole thinking about health security has to change. The concept of every country trying to look only within its own borders is completely, mindbogglingly, a waste of everybody's time.

THINK GLOBAL HEALTH: The WHO has put out a call for $675 million to support low- and middle-income countries in mobilizing response to COVID-19. They've only received $1.2 million so far. How important is it to you that WHO and international efforts are appropriately resourced in addressing this crisis?
IHEKWEAZU: The WHO is so necessary in the world today to enable [a collaborative response], and there are very few other institutions other than WHO and African CDC that can make that happen. So we are very supportive of the work and the solicitations from WHO so that we can have a collective approach.
We lost, to a large extent, the collective will to respond together
It's unfortunate that many countries that we look up to—actually we have looked up to for years—were the first that broke out of the framework of the international health regulation that countries collectively agreed to once there was a sense of a problem in China. We lost, to a large extent, the collective will to respond together. So from my perspective, and I think this view is shared by many of my colleagues on the continent, we do appreciate some collective thinking, and we do appreciate the platform that WHO provides to do this. What we would all like to see a little bit more of is that once that thinking happens, that more countries on the continent—now this is almost a criticism of ourselves—develop organizations like we have, the Nigerian Centers for Disease Control.

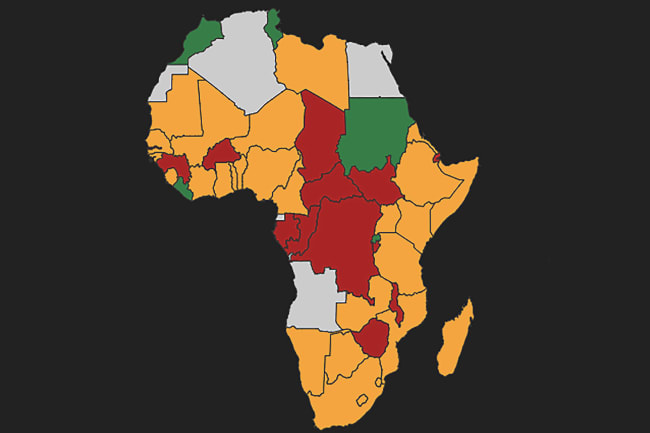
Many African countries have not done this and still rely on the bureaucracy within ministries of health to manage health security crises, and this is completely inappropriate in the world of today. This is really what we need on the continent, for the technical institutions, national public health institutions, to be empowered to grow their capabilities to do the technical work and leave the bureaucracy and the political measures to our colleagues in the ministry while the experts deal with the response activities and advising populations on what to do when there is a crisis.
□ □ □ □ □
THINK GLOBAL HEALTH: One thing that has changed since the Ebola outbreak is the establishment of the Africa CDC. How have they been mobilized in response to COVID-19?
IHEKWEAZU: Africa's CDC has been great in terms of pulling countries together to work together on specific areas. But how they have done this, too, is not by being this cathedral that sends down messages to the masses. Rather, what they have done is used capabilities within Africa to—where there are strengths—to support the development of that area in other parts of the continent.
Our reality is we don't have those resources. So what do we need to be safe versus what can we afford—and what is the appropriate midpoint for us?
Nigeria is leading on the infection prevention and control pillar. Just last week we hosted a training workshop here for other African countries to agree on a framework of what level of [infection prevention control] can we provide in our context that is safe enough, but also considering our socioeconomic reality. These are not easy questions to answer because once you watch TV and you see everybody dressed in hazmat suits, you automatically assume that that is what is necessary to deal with this. Our reality is we don't have those resources. So what do we need to be safe versus what can we afford—and what is the appropriate midpoint for us? So we've been working on that figure on behalf of Africa CDC for the continent.

Africa CDC has been an incredible addition to the health security architecture that we have on the continent. Every week we have teleconferences among the leaders across the continent, sharing information, sharing the progress. You know, we never had this during Ebola. Maybe that's the reason why that outbreak grew out of hand as quickly as it did.
□ □ □ □ □
THINK GLOBAL HEALTH: Nigeria has a robust oil and gas industry, which has significant exposure in an outbreak like this. How much are you working with the private sector, and is it enough?
IHEKWEAZU: The lessons from the Ebola outbreak is, everybody becomes interested when there's a crisis… If there's one good thing that I hope will come out of this coronavirus outbreak, it is an appreciation across society of the potential impact that a single virus has on the bottom line of companies—not to talk about on the health of humans.

[COVID-19] is a big problem. I think it demonstrates to the world that we have to take global health security seriously and deal with it as a security and socioeconomic threat, and not just a health threat. As long as we conceptualize this as a threat only to health, the response will remain within people in the health sector, and in many countries in the world, most people in the health sector don't have sufficient influence and power to make decisions about resource allocation.
We know what to do. We know how to do it. But we don't have the resources necessary… to keep the world safe.
And it is our resource allocation that will ultimately lead to our ability to develop the countermeasures that we need as a world, as a global community.
So I hope that this kind of shakes up enough people to bring in enough interest from the bigger players that need to come together to support the development of the work that we need to do. We know what to do. We know how to do it. But we don't happen to have the resources to develop the skills necessary to do the work that we think we need to do to keep the world safe.

THINK GLOBAL HEALTH: How do you prioritize and mobilize your resources, your people? What sort of choices do you have to make on a day-to-day basis?
IHEKWEAZU: We had and still have what I'd call a big diagnostic insufficiency in Nigeria. In many settings you would expect routine laboratory services to make the appropriate diagnosis of patients, and then only inform public health when they've detected a new case of a particular infectious disease or a cluster of cases.
Because our diagnoses were [previously] so poor in Nigeria, our first real challenge was to improve our diagnostic abilities so that all those things that were being wrongly diagnosed as resistant malaria, or just not diagnosed at all, we could then identify what these things were.
Two hundred million people, with one of the highest population densities in the world, living in the middle of the tropics. If I were a virus…
Of course, once we did that, and started looking a lot harder, we started finding all this spectrum of infectious disease that no one had found in Nigeria. We found the first case of yellow fever in over seventeen years, the first case of monkeypox in over thirty years. Right now we have the largest outbreak of Lassa in history—every year we report more cases. So, in a way, what has happened is the more we've improved our own systems of surveillance, awareness, detection, laboratory confirmation capabilities, we found all these more cases and brought them to light. And that has inevitably meant that every week we have a team or several teams—often in different parts of the country—supporting the response to one cluster of cases or another. And many of them no one ever hears about.
We are two hundred million people, with one of the highest population densities in the world, living in the middle of the tropics. If I were a virus, there is no better place than Nigerian context to grow. So as the viruses grow or emerge and compete for space, we have to also have the capabilities to respond.

THINK GLOBAL HEALTH: Tell us a little bit more about the Lassa fever outbreak: its history, what you're doing to get it under control, and where things are going?
IHEKWEAZU: When people think of Lassa, they think about the end-stage bleeding syndrome. The fact is that syndrome happens in a small proportion of cases, and only the most severe ones. So most people present like a normal fever. And for a long time, we didn't even have the capability of making that diagnosis. So we focused on building laboratory capacity, and what we have seen is in the areas where it's most endemic, we've actually built a fairly strong response architecture.
For a long time, we didn't even have the capability of making that diagnosis, so we focused on building laboratory capacity
One of the issues with Lassa is the labs are fairly complex labs. Even though we have pushed on building new labs, we still have [only] five labs in Nigeria—big country. So we worked with a private company to organize specimen transportation, transporting the specimens from wherever they're collected to one of these labs. By doing that, we've really increased our capacity of getting the samples, testing them, and providing results. In a way, we are finding more cases, and in the areas where we've found the most cases, the expertise to manage these cases has improved. This year we found a new cluster of cases in Kano, a cluster of cases among physicians—surgeons. Four people who were operating on the same individual got infected. Two of them passed away. And there was a lot of panic in Kano.
We had to go in, reassure them, because Lassa was new to them—they didn't know what to do. So really, whenever there's a new case in a new part of the country, there's often a lot of anxiety, and we have to go in and manage that.

When you're dealing with a disease where there appears to be no hope, no interest, and no attention, it's a very devastating situation for health care workers to work in. What has changed over the last few years is by bringing this to the attention of the global health community and saying: Listen, we have this viral hemorrhagic fever with a case fatality rate of about 20 percent that nobody's paying any attention to. We hosted a big international conference in February of last year, brought this to the attention of at least those interested in infectious diseases, and we have stimulated a whole series of recent efforts towards new therapeutics and new vaccines.
Do I deal with 600 cases of Lassa or focus on COVID-19? The reality is, I can't choose between either of those. We've got to be prepared for both.
While we're still waiting obviously for this research to come through, the health care workers are much more motivated to do the best with what they have when they know that the effort is being made to develop medical countermeasures that are providing hope in the future.
So on the one hand, we have this big challenge of a zoonotic infection that leads to so many cases and deaths. On the other hand, we have to deal with every other thing being thrown into our path—like corona[virus] at the moment.
To me, right now, it's a big struggle. Do I deal with 600 cases of Lassa so far just in the first two months of this year? Or do I focus on preparedness for this new respiratory virus that no one yet knows what will happen if transmission establish itself in one of our countries. The reality is, I can't really choose between either of those. We've got to be prepared for both.

EDITOR'S NOTE. This interview was conducted by phone. What is printed here was taken verbatim from the transcript but edited slightly for length and clarity.