The pace of COVID-19, the ongoing novel coronavirus outbreak, has been astonishing, and it is inevitable that this will become a pandemic, if it hasn't already. When a disease is a pandemic, it considered to be an ongoing threat to people around the world. The virus has already spread widely, has not been contained in many areas, and there have been unlinked chains of transmission in multiple countries. There are undoubtedly many more cases in many countries; an estimated two thirds of COVID-19 cases exported from mainland China may have remained undetected.
Fortunately, we have the lessons of pandemic influenza, which can guide our actions. A framework allows for initial and ongoing assessment of how infectious and severe a virus is, which informs decision-making. Applying pandemic influenza frameworks to COVID-19 can help estimate impacts and identify appropriate mitigation strategies, including non-pharmaceutical interventions.
This suggests a moderate or severe pandemic
Although data on COVID-19 is sparse and marked by substantial uncertainty, the disease is currently somewhere between 3 and 5 on a five-point scale for transmissibility, and between a 3 to 6 on a seven-point scale for severity. This suggests a moderate or severe pandemic, as shown below.
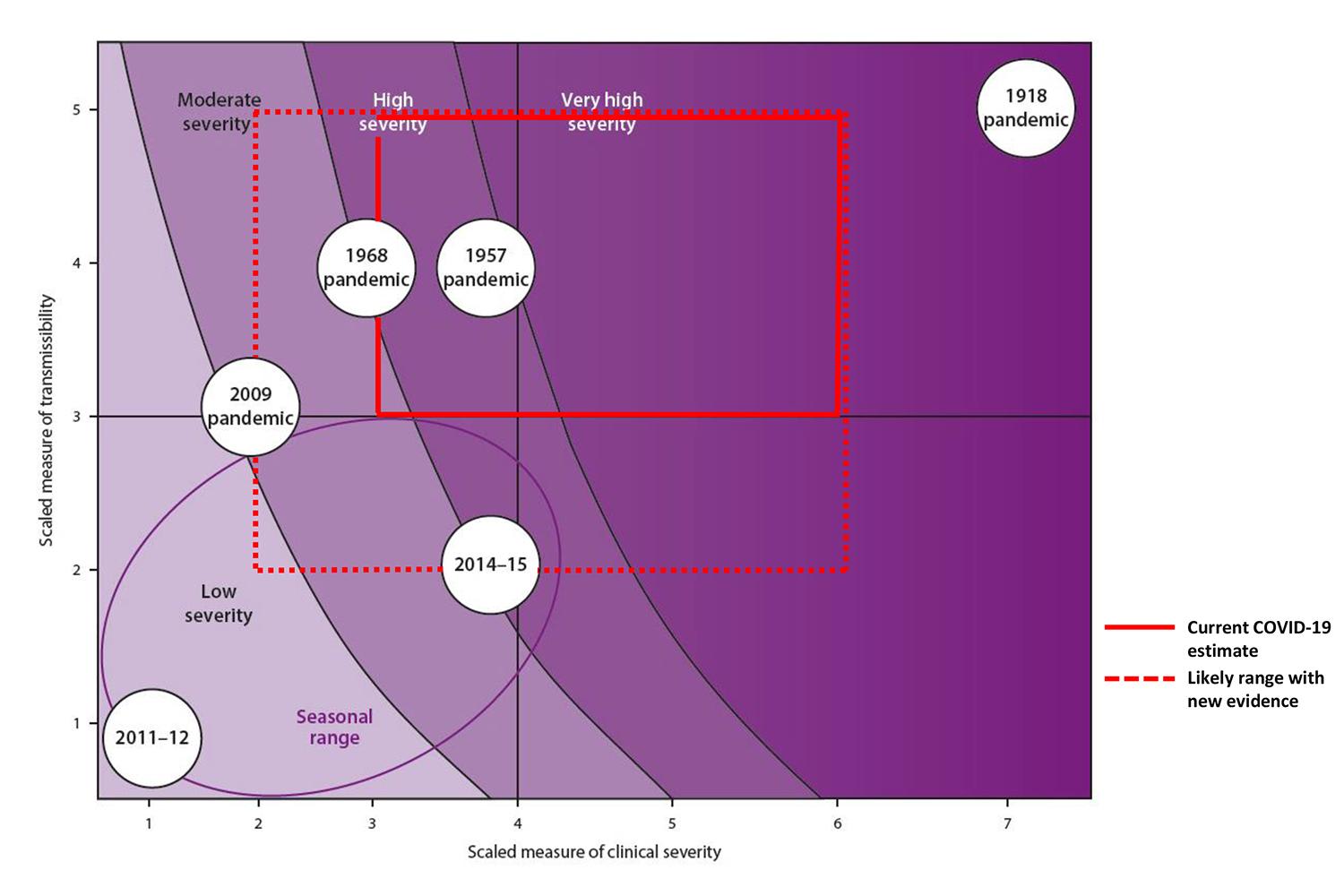
As the pandemic progresses, more accurate categorization will be possible. The most recent comparable influenza pandemics may be H2N2 in 1957 and H3N2 in 1968, which resulted in some 1.1 million and 1 million deaths worldwide, respectively, but in a much different global context. Vaccines and medications can be developed more rapidly than half century ago. Intensive care is more effective now, but today diseases can have greater impact due to increased travel and urbanization, larger populations of older people and those with comorbidities, and wide disparities between the most and least prepared countries in the world. Although there is now more timely access to information, there is also faster spread of misinformation.
Finding What We Don't Know
However, the application of this framework to COVID-19 is limited by a lack of robust information on transmissibility and severity. Transmission estimates may be inflated if secondary cases arise from unrecognized index cases and underestimated if mild or asymptomatic secondary cases go undiagnosed.
To better understand transmissibility, detailed epidemiologic investigations should be undertaken in countries when the virus is first identified
Publicly available measures of transmissibility based on the estimated basic reproductive ratio (R0) are between approximately 1.4 and 3.3, which means it is probably more contagious than seasonal flu but is much less when compared to something like measles. To better understand transmissibility, detailed epidemiologic investigations should be undertaken in countries when the virus is first identified, including studies of its "attack rate" in households, schools, health care facilities, and community at large. An accounting needs to be taken of all outpatient visits for any flu-like illnesses, and how many people carry the virus over time in communities with known COVID infections.

Our current understanding of how severe COVID-19 is may be overestimated, since it's easier to detect people who are suffering severely than mild or asymptomatic cases. Some of the available measures we can apply to assess its severity include case-fatality ratios, deaths-to-hospitalization ratios, and the proportion of intensive care unit (ICU) admissions.
What we know now, we believe to be inaccurate
Again, what we know now, we believe to be inaccurate. The documented COVID-19 case-fatality ratio of 2-3 percent is likely an overestimate. To correct for errors in underreporting of mild cases and the time lag between cases and deaths, we can use a different measure known as the infection fatality rate. This is the proportion of all people with infections who die from them, which the WHO estimated at 0.3-1 percent for COVID-19. One estimate of deaths-to-hospitalization was documented in a single-site review in which 6 out of 138 (4.3 percent) confirmed patients died. In the same study, 36 out of 138 (26 percent) required ICU care. These estimates are based on a small number of patients, and future estimates are likely to be more accurate and generalizable.

How do we move forward? To accurately ascertain disease severity, we should establish longitudinal studies that monitor the outcomes of infected patients, stratifying by variables such as age, sex, and medical comorbidities. In places around the world that have the advantage of strong public health programs, we should establish surveillance to track trends and impact of these variables on overall mortality.
How Differences in Severity Would Play Out
In a best-case scenario, the pandemic would affect only 1 percent of the global population, with an influenza-like case fatality ratio of 0.1 percent. A COVID-19 pandemic like that would still tragically cause thousands more deaths, but a far greater human disaster would be avoided.
A worst-case scenario with a more transmissible and severe coronavirus would affect 10 percent of the global population with a case fatality ratio of 1 percent, causing millions of deaths. Probably the truth lies somewhere in between. Current evidence suggests that COVID-19 will become a moderate or severe pandemic. Even though there is likely little or no population immunity to the virus (named SARS-CoV-2), with proactive planning and implementation, the impact of this pandemic can be mitigated to avoid the worst-case scenario.
That planning should start by looking back at the pandemic influenza plans and rapidly adapting them to prepare for and respond to a COVID-19. Countries, states, and communities need to prepare to implement individual, health care, societal, and pharmaceutical countermeasures.
Proven treatments are likely months away, and effective vaccines are at least a year away, so near-term strategies should focus on mitigation of health, economic, and societal impacts. The core of this strategy is to implement non-pharmaceutical interventions— especially in at-risk groups and those with limited access to care and services—to reduce the number of people infected.
What do these non-pharmaceutical interventions look like? They include things like covering your mouth when you cough or sneeze, hand hygiene, and voluntary home isolation when a person is sick. It also includes routine cleaning of frequently touched surfaces at home, work, schools, and in health care settings. A big part of implementing these interventions is education—communicating frequently and effectively to the public and training workers on how to reduce the spread of infection.

We must also consider when to add more disruptive personal and community non-pharmaceutical interventions, including voluntary home quarantine for entire households and mandatory use of face masks by people who are ill. Containing or mitigating COVID-19 may necessitate school closures, cancellation of mass gatherings, mandatory teleworking, and other social distancing measures.
If not communicated properly, community non-pharmaceutical interventions can lead to fear, stigmatization, violence, and mistrust in government, media
Specific non-pharmaceutical interventions may vary by location but effectiveness depends on appropriate implementation.
Why?
These measures are unfamiliar, difficult to enforce, and can cause significant disruption. Engagement and communication around their use will be vital to effective implementation. If not communicated properly, community non-pharmaceutical interventions can lead to fear, stigmatization, violence, and mistrust in government, media, and health care institutions, and adherence to recommendations can be low.
Practical tips are also important to convey, including planning for extended periods at home by requesting long-term supplies of medications, accessing telemedicine services, procuring essential items, and connecting with vulnerable friends and family to ensure they are supported. Personal and business travel decisions should be delayed as long as possible, since better information will lead to more informed decisions. Businesses should develop plans to maintain critical operations if staff are sick or unable to work. Health care facilities should prepare to safely identify and treat a surge in both mild and severe cases, protect staff, and ensure capacity to treat severe cases, all while maintaining basic health care services.

At the national and global level, work must continue to strengthen core systems to find, stop, and prevent health threats. This includes improving timely case detection and critical care for the most severely ill patients. Countries should also share all data and information on their progress to help preparedness in countries experiencing later waves of illness.
Billions spent in preparation would save hundreds of billions spent in response and may save millions of lives —perhaps even prevent the next pandemic
Funding to support COVID-19 operations at WHO has been inadequate, and a U.S. $2.5 billion proposal by the Trump Administration for COVID-19 pales in comparison to prior U.S. appropriations for the much less severe health threats of H1N1 influenza ($7.6 billion) and Ebola ($5.4 billion). COVID-19 is a sobering reminder of the value of investing in preparedness. COVID-19 has affected some of the most prepared countries in the world, and has yet to take hold (as far as we know) in countries least equipped to deal with it. To address gaps in global health security and end the cycle of panic and neglect, tens of billions of dollars must be urgently mobilized to mitigate the effects of COVID-19.
For an investment of approximately $1 per person per year in lower income countries—a small fraction of the hundreds of billions of dollars in economic costs already attributed to COVID-19—the world could both better respond to the impending pandemic and prevent the next health crisis. Billions of dollars spent in preparation would save hundreds of billions of dollars spent in response and potentially save millions of lives —perhaps even prevent the next pandemic.
COVID-19 is a historic global health threat and a pandemic seems inevitable. Disaster, however, is not. Our preparedness is critical to saving lives and mitigating health, societal, and economic impacts, and the steps we take now are of utmost importance.













