Soon after I became director of the U.S. Centers for Disease Control and Prevention (CDC) in June of 2009, I was asked to brief President Barack Obama about the emerging pandemic of H1N1 influenza. It was the first time I had briefed the president, there was a blizzard of information from CDC’s experts, and I had a videocall with dozens of CDC professionals—most of whom didn’t know I was about to brief the president—just before the briefing to make sure I had the latest information. It was still unclear how severe this strain of the virus was, though initial data from Mexico suggested that it could be bad.
The president asked me, “We’re not going to see a million deaths in this country, are we, doctor?”
I replied, with more certainty than I felt, “No, Mr. President, we won’t.” If asked the same question today about the novel coronavirus, I would have to reply, “I hope not, but that’s a possibility.”

Public health is crucial to both understanding and guiding the response to health threats. But if public health officials can’t do their jobs—because they’re distracted by the complex problem of cruise ships, or quarantines, or public perception—all of society suffers.
We need to learn more, inform public and the media more, and let the best and most current data guide our actions and our statements
During the three major emergency responses I oversaw at CDC in the past decade—H1N1, Ebola, and Zika—CDC and state and local health departments were able to learn quickly and act quickly to protect people. The COVID-19 pandemic is an unprecedented threat—never before has a new respiratory pathogen been identified then spread around the world. And as with those responses, public health must lead this response. We need to learn more, inform public and the media more, and let the best and most current data guide our actions and our statements.
To act effectively, we must set priorities. Even if there were unlimited financial resources, human resources are limited. And if our most precious human resource—specialists who can help figure out how this virus is most likely to spread and what works best to reduce spread—are busy with lower-level priorities, no one is well served. For example, CDC staff should not be asked to manage any component of quarantine – other parts of the Department of Health and Human Services can do that, with CDC technical guidance. The CDC must be free to do what it does best: figure out how the infection is spreading and how best to reduce the spread.

What makes us think that COVID-19 could potentially cause a million deaths, and what can we do to reduce the potential impact?
Worst-Case Scenario: A Million Deaths in the United States
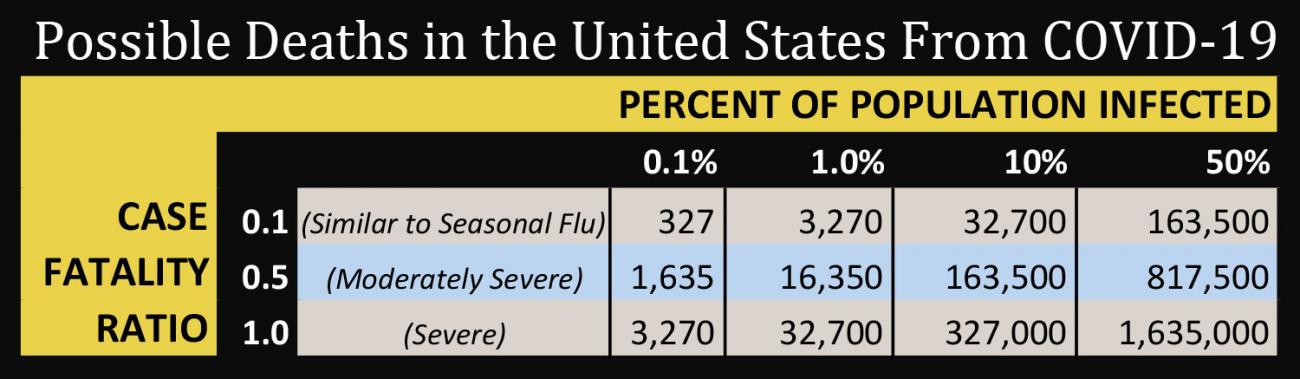
The table below shows what would happen in the United States in a worst case scenario—but unfortunately one that’s not implausible. In this scenario, half of the U.S. population would get infected with COVID-19 and more than one million people would die.
It’s likely that the case fatality rate is below 1 percent, and it’s possible that aggressive action could minimize the impact of the virus in the United States. But we need to plan for the worst and work for the best.
How to Work for the Best-Case Scenario
The understandable concern of political and other leaders has led to a focus on cruise ships, travel bans, and testing – important issues, but not interventions that will drastically reduce spread. Focus on these issues are making it harder for public health specialists to do what is already an extraordinarily difficult job. When the virus first enters a community, extensive efforts are needed to find cases, isolate contacts, and stop spread. But when there are multiple cases, it’s time to shift to broader measures to reduce risk.
When there are multiple cases, it’s time to shift to broader measures to reduce risk
The United States has particular vulnerabilities. Not everyone has paid sick leave or access to health care. We already had an unacceptably a high number of hospital-acquired infections before coronavirus started spreading here, increasing the risk that health care workers and patients will get infected in health care facilities. And each state and community is diverse, with unique barriers to—and strengths in—the response.
Here are the top ten actions we should take to reduce the risk a million people in this country will die from this pandemic:
- Protect all who are vulnerable. For those with underlying conditions and older adults, increase social distancing—limit the number of people who come within six feet. Ensure that those who do have come into contact with them are not ill.
- Stop all non-essential visits to nursing homes and other long-term care facilities for the near future. The risk is too high.
- Accelerate work on effective treatments and vaccines. A vaccine could take one to two years to develop, and its success is far from certain, but we must try. Treatments could become available sooner, and they may increase survival for people who are infected—and, ideally, prevent some infections in people known to have been exposed. It’s time to start planning for distributing these treatments and vaccine if they become available, as they become available.

- Cancel large gatherings, with the exception of geographic regions and populations not experiencing community transmission. Making that hard decision now could mean the difference between thousands and tens of thousands of infections in a community. If mass meetings do occur, older and medically vulnerable people should not attend.
- Protect our health care workers and our health care system. This means improving infection prevention and control, preparing to safely surge to care for an influx of patients, anticipating and quickly attending to the “worried well” and those with mild illness including people who flood health care facilities concerned their minor symptoms are COVID-19, making sure patients have a three-month supply of critical medicines such as those for diabetes, hypertension, and seizure disorder, and ensuring that hospitals have the ability to increase their capacity for intensive care, including for those needing ventilators.
- Stop handshakes, and opt for a wave or namaste instead; cover your cough, and wash hands often.
- Don’t go out if ill. Let’s encourage our digital streaming services, including Netflix, Disney, Hulu, Apple, Amazon and delivery services to offer free services to people on home quarantine and in places with community transmission in order to make staying at home more pleasant—and therefore increase the chance people will comply.

- Telework if spread may be occurring in your area.
- Assess school closure. There are costs and benefits for each measure that we take. Closing schools can help during an influenza outbreak because children are a major source of the spread of influenza. We don’t yet know if children are a major source of the spread of this virus. We do know that closing schools can be disruptive—not only because of the educational impact, but because of the impact on families and on the many services schools provide.
- Learn more as fast as we can. We learn more about how this virus spreads and how to stop it every day. We still need to learn how deadly the virus is and exactly how it spreads and how best to limit spread and reduce deaths. As we learn, we will inevitably need to adjust our actions.
Speed matters—a lot. It’s been said that a week is a long time in politics. With COVID-19, a week is not a long time, it’s an eternity. The sooner we act, the more we can decrease the likelihood of a million deaths in the United States. Clear, consistent communication from credible sources builds public trust and saves lives. When faced with a scenario in which so many Americans could die, there’s no time for politics.


