Worldwide, more than four million people are believed to live with sickle cell disease, a genetic disorder that alters the normal function of red blood cells and causes lifelong health problems. The vast majority of people with the disease live in Africa, the Middle East, and India. Despite its disabling effects—which can include severe pain, susceptibility to infections, and fatigue—it gets less attention than it merits.
Lea Kilenga Masamo is trying to change that. A 32-year-old from Nairobi, she has spent the last eight years raising awareness about the non-communicable disease (NCD) and advocating for the Kenyan government to better meet patients' needs. She spoke about her work and how it changed during the pandemic.
□ □ □ □ □ □ □ □ □ □ □ □ □
Think Global Health: Tell me a little about your experiences as a person living with sickle cell?
Lea Kilenga Masamo: Sickle cell is a genetic disorder that changes the shape of the round normal red blood cells into deformed crescents, which become trapped in the blood vessels and create blockages that reduce oxygen transportation to organs. This can induce severe pain, particularly of the bones, and it eventually culminates in organ damage. Later in life, people like me experience heart failure, lung failure, brain failure, and kidney failure. Sickle cell also affects growth and intellectual development, which impacts things like schooling, employment, and mental health. So, it's a lifelong illness and each life stage—childhood, adolescence, and adulthood—brings its own challenges.
Think Global Health: When did you become aware of your illness?
Lea Kilenga Masamo: I didn't think it was abnormal. We lived in a family where two of my older sisters also had sickle cell. I didn't realize that not every child in the world took medicines every day or went to the clinic every so often, like I did. When I was 13, a boy in our class brought up the fact that my eyes were jaundiced—my eyes have this yellow tint—and it was peculiar. I hadn't noticed before, and I became curious, and then my parents broke it down for me.
Sickle cell is a stigmatized illness. It's a genetic disease, which has this connotation of witchcraft and ancestral curses. And it wasn't really talked about. Grown-ups used to treat me differently, as if it were this very terrible or difficult disease that you do not have a chance of surviving. Most of the people who had sickle cell back then didn't survive, and 50 to 80 percent of deaths are in children under the age of five.

Think Global Health: How did you become interested in advocacy?
Lea Kilenga Masamo: It essentially came about from frustration. I decided, I'm not the only one who lives with this disease so let me go and take photos and talk to people about their experiences with sickle cell.
It was just a hobby at first. I went to the bigger hotspots for sickle cell—western and coastal areas of Kenya—and I was dumbfounded by the difficulties, the sadness, and the hopelessness that I saw. Children who were 18 looked like they were four years old and breathing their last breath. A mother with three children with sickle cell who told me, "My husband has abandoned me because he says this disease is not in their family so I must have cheated on him." A family that says that one of their children has sickle cell so they don't send him to school, they just lock him in a room because why should they bother spending money when the child is not going to survive?
It was really hard. I wasn't prepared for that. I thought I had it bad… but the people I met had it worse. A lot of people had complications—strokes, necrosis of the bones, brain damage, conditions that shouldn't have reached such a severe level if basic care was available. So, I had to stop and come back home to Nairobi and reassess my life. I was haunted, and I sought to do something, and that's when my work started. That was eight years ago.
I'm not the only one who lives with this disease so let me go and take photos and talk to people about their experiences with sickle cell
Think Global Health: What kind of activities did you undertake?
Lea Kilenga Masamo: Throughout my initial journey I raised awareness in the media, and at any kind of NCD conference. The ministry of health and different stakeholders used to invite me as a patient advocate. I'd stand outside with my small booth with all the photos and all the stories. And that's how I built my credibility and built my initiative and also built a sense of urgency for sickle cell.
Because health care in Kenya has been decentralized, you can only do so much at the national level. I was advised to go create change in a small place that is scalable and can be replicated in different areas that have high sickle cell burden. That's why I moved from Nairobi to Taita Taveta [in southern Kenya]; I've been there since 2018.
Taita Taveta is one of the counties in Kenya with a high burden of sickle cell. And it's also a marginalized area with a lot of inequalities in education, health care, access to water, food. Most of the people live on less than $1 a day. So non-communicable diseases are largely neglected, not because we don't want to do anything about them but it's just that the problems on the table are many—from female genital mutilation to HIV, to diabetes and hypertension, to very low levels of education, to sickle cell.
I started a non-profit organization called Africa Sickle Cell to provide access to care for people with sickle cell. We do not duplicate the role of the government, we bring partners on board to support health systems development and infrastructure development with regards to the clinic space itself—diagnostics, training health-care providers—and establishing a clinic within the local hospital so that patients living with sickle cell can have a place to go. We supported the creation of two government-run clinics here; one is funded by the Novo Nordisk Haemophilia Foundation, the other one is government supported. We have essential medicines on the shelves. We just got diagnostics. And most of the people who live with sickle cell there are provided with health insurance through the organization.

Think Global Health: How did the pandemic affect life with sickle cell in Kenya?
Lea Kilenga Masamo: Last year gave me a reality check on the priorities of global health, in terms of who is at the table, who is not, and what people like us need to do to get a seat at that table. If you're not able to access these platforms, if you're marginalized—geographically marginalized or educationally marginalized or financially marginalized—then you have very little opportunity to get yourself heard.
In Kenya, for a person living with sickle cell but also other non-communicable diseases, it was difficult to access medicines. Because there was no movement of anything, cross border supply chains were disrupted and there were severe delays. So, you could not get medicines for specific conditions at the quantities that you would like. And there was very limited stock; and once you ran out, then you had to wait four or five months for that to be resolved. And for people with chronic conditions, you cannot wait that long, unless you stockpile medicines, but medicines expire.
"Last year gave me a reality check on the priorities of global health, in terms of who is at the table, who is not"
The media was focused on counting numbers on COVID and nothing else. So, we had to essentially come together as people living with non-communicable diseases in Kenya. We were able to speak to the Ministry of Health and were included in the Non-Communicable Disease COVID-19 Response Committee. And we were able to advocate for non-communicable disease clinics, point of care centers, and medicines. International and local organizations came in, based on the lived experiences of people like us who would share stories of what is actually happening on the ground.
Private companies came on board to support people with non-communicable diseases so that they could afford medicines. Nowadays, the area that I stay in, this very marginalized area, is one of the few areas in Kenya that has sickle cell medicines on the shelf. And most of the people who live with sickle cell, or the households with a child that has sickle cell, we have put them under health insurance so that they can get this medicine and care for free.
Think Global Health: What changes did the government implement due to your advocacy?
Lea Kilenga Masamo: When the pandemic started we were not able to access hospitals where the government had restricted movement due to COVID-19; we were not able to access clinics; we were not able to access medicines. So, the change brought about by our advocacy measures was that they were able to open up these hospitals and special NCD clinics within specific catchment areas, and to provide medicines to people living with NCDs.
The government also realized that people living with NCDs are key stakeholders, and that they should address the concerns of people with lived experiences. So, the process that started then is now being incorporated into the Non-Communicable Disease Prevention and Control Strategy of 2020 to 2025.

Think Global Health: What are the most important changes you would like to see in how our society treats sickle cell disease?
Lea Kilenga Masamo: It still hasn't been prioritized globally. The biggest burden is in sub-Saharan Africa, and that's why I think it's lagged behind. Most of the interventions for sickle cell are copy-pasted from the West. And rather than being led by Africans or by members of the Global South, most of the priorities and agendas are led by the Global North. And our priorities are left unheard.
There's a lot of inequity. There's a missed opportunity for countries and communities that are affected with sickle cell to mobilize together and provide a unified response to this disease. Most of the time, unfortunately, African governments wait to be led by the World Health Organization (WHO) or by the West and we miss the opportunity to mobilize our own communities toward specific agendas that affect us. It is quite astonishing, but there is no country in the world that has a sickle cell policy in place, including countries with a high burden of sickle cell.
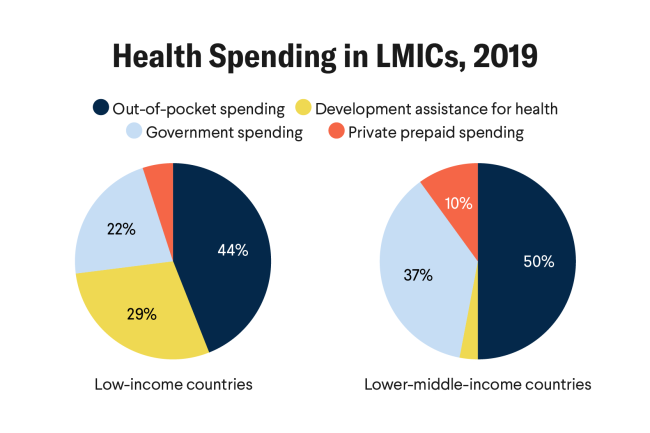
What financial systems have we put in place to safeguard expenditures on sickle cell? How have governments strengthened their systems to be able to ensure that sickle cell care is affordable, accessible, and available to all? How do we ensure there is early diagnosis for sickle cell—when you diagnose early you're able to intervene and cut unnecessary deaths.

Think Global Health: What are some elements you can imagine including in a sickle cell policy?
Lea Kilenga Masamo: It should be patient-centered: how are we responding to sickle cell in a way that is inclusive of patients, and how do we tailor services that are responsive to patients' needs? A sickle cell policy will be multi-sectoral: what role do education, agriculture, and ministries of youth and sports and labor play in the management of sickle cell? Sickle cell affects education severely—you have intermittent schooling, you can't go to school every day because of sickle cell. So do we have special [educational] considerations for people living with sickle cell who have intellectual deficiencies? A sickle cell policy would ensure there's a facility in every burdened county, so people can be diagnosed early. It would ensure basic essential medicines are available at the primary health centers, and there are community engagement programs to address community stigma. Blood is an essential commodity but if we do not have blood and blood components that are available, accessible, and affordable in the very marginalized and primary health centers, then management of sickle cell is not possible.
Think Global Health: What do you think is sometimes misunderstood or misconstrued about the experience of having sickle cell?
Lea Kilenga Masamo: The media under-reports sickle cell, in my opinion. A lot of the stories perpetuate a specific societal stigma. And there's a dearth of stories that include the voices of persons living with NCDs, of people doing amazing things in spite of living with sickle cell. Sickle cell is not an automatic death sentence. When you detect it early, when you manage it properly and without interruption due to financial constraints, people living with sickle cell have a chance of achieving their fullest potential.
"How are we responding to sickle cell in a way that is inclusive of patients, and how do we tailor services that are responsive to patients' needs?"
Think Global Health: Where have you spent this last year?
Lea Kilenga Masamo: Actually, I've been in Rwanda for school. I enrolled last year at the University of Global Health Equity. I got my acceptance letter last year in the middle of the pandemic, and I started school in October, online and then on campus in January, and we're about to graduate. After school, I plan to go into research. I want to find out what's working, what's not, and what gap we need to focus on. I also want to apply for a PhD in medical anthropology at Harvard. A lot of people are doing advocacy and programs and there's so many solutions on the ground, but very limited research on evidence-based practices of what works with regards to responding to sickle cell.

EDITOR'S NOTE: This interview was conducted via telephone and has been edited for length and clarity.